Reauthorizations are a constant part of ABA therapy because insurance approvals usually cover only a set number of hours or a fixed time period. Missing a reauthorization window can disrupt services for families and cause billing delays for the clinic. Automating reminders makes the process more reliable and less dependent on staff remembering every deadline.
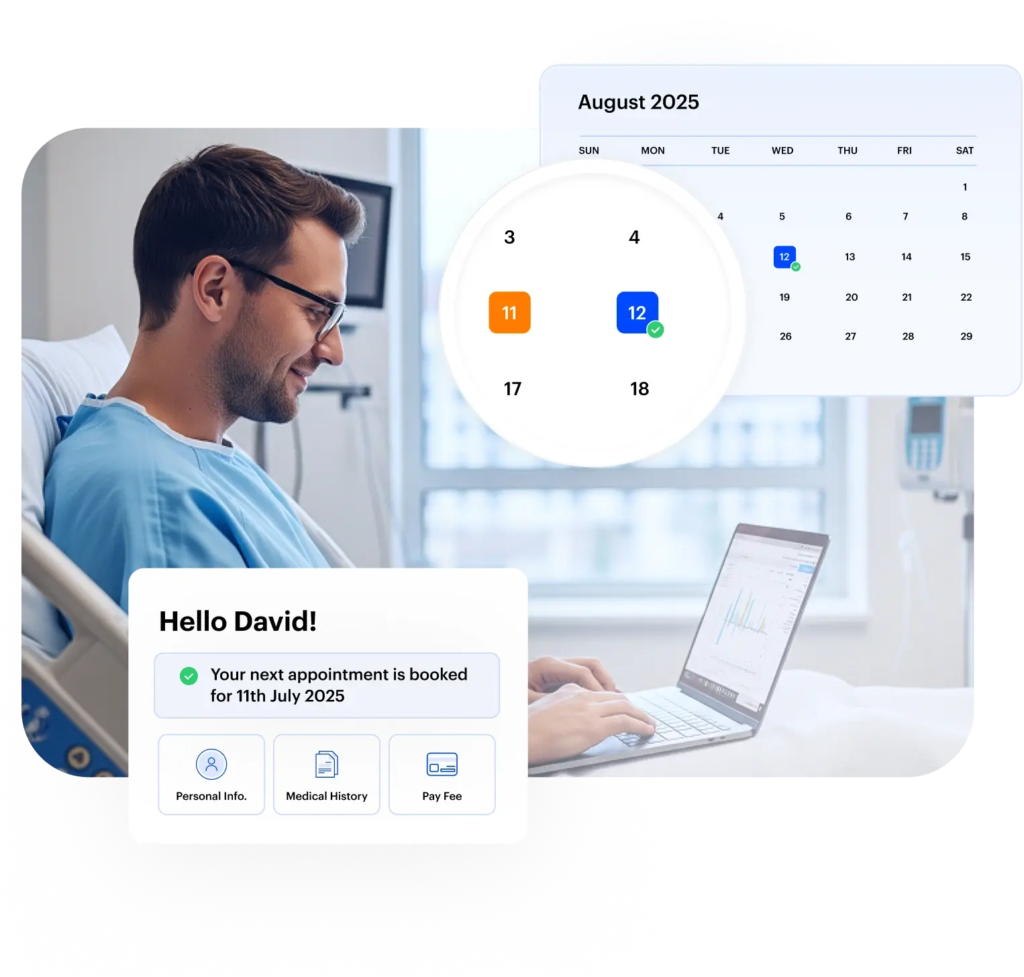
The first step is tracking the right fields in your ABA practice management system. For each patient, capture details such as authorization start date, end date, total approved hours, and hours used. With this data in place, you can build rules that trigger reminders before the authorization expires or when usage reaches a certain threshold.
Automated reminders can be set up for both staff and families:
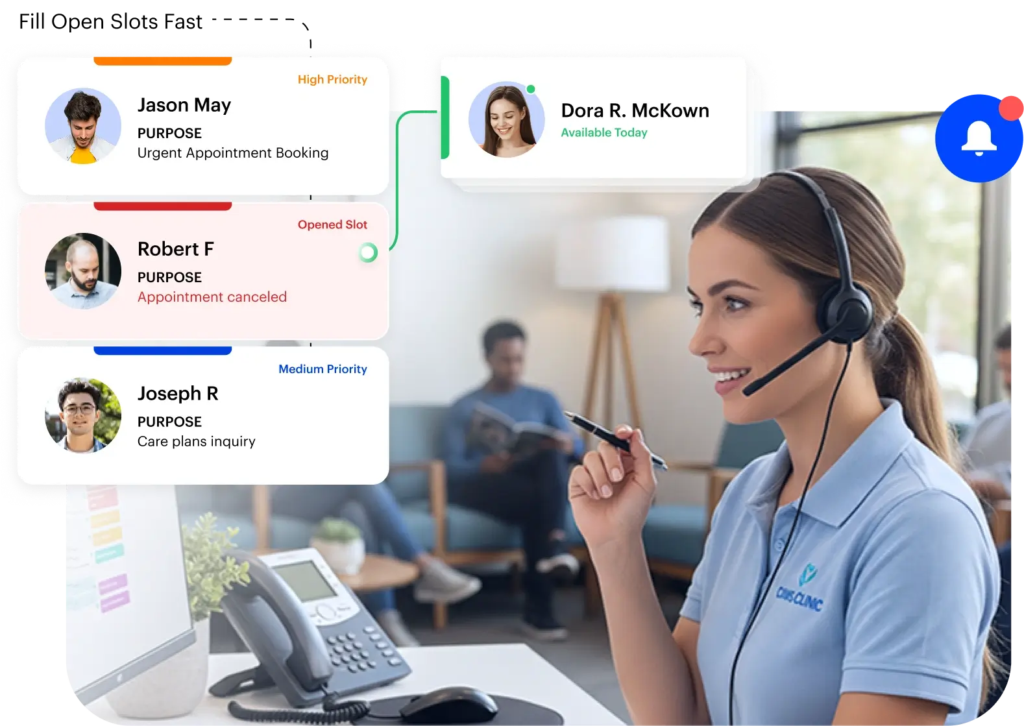
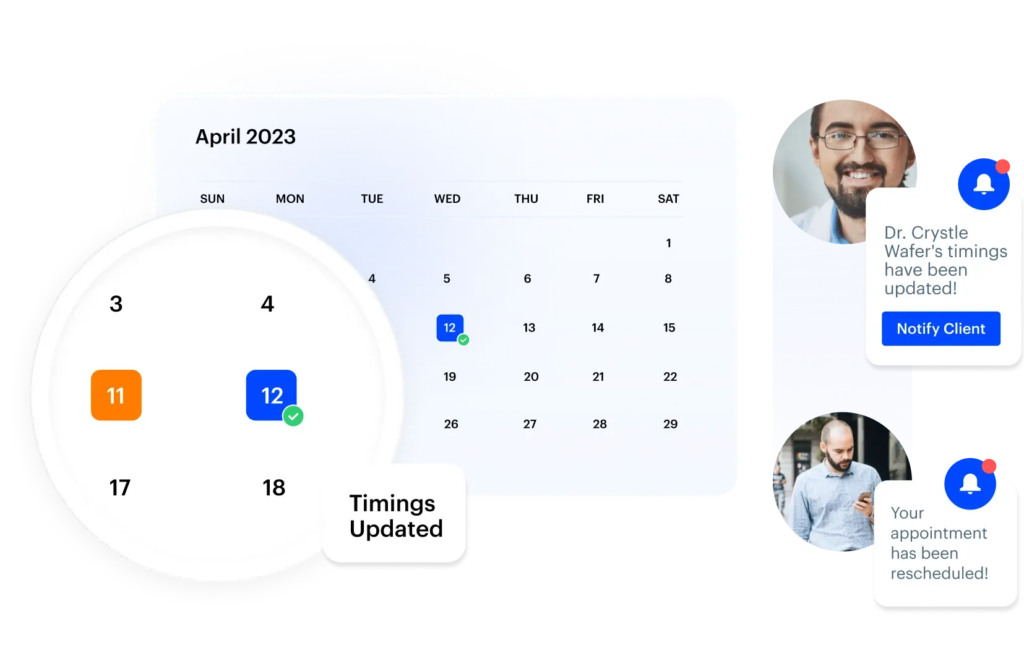
- Staff reminders: Send internal notifications to intake coordinators, billing teams, or clinicians when a patient’s authorization is approaching expiration. For example, you might send alerts 30 days, 14 days, and 7 days before the deadline. These reminders can automatically create tasks like “Prepare reauthorization paperwork” or “Submit request to payer.”
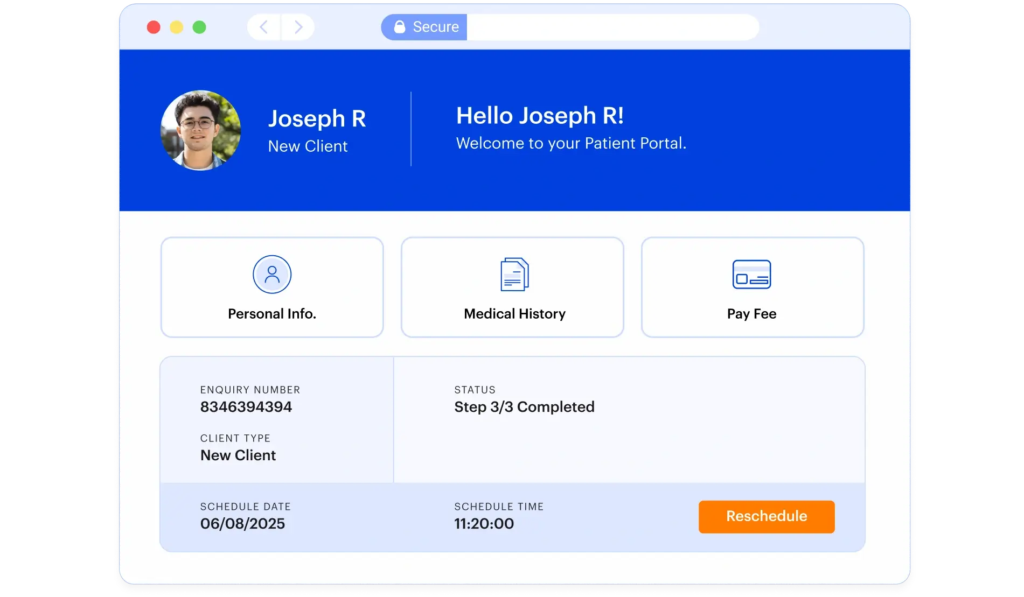
- Family reminders: Families can also receive automated communication letting them know a reauthorization is due, along with instructions on what they need to provide—such as updated reports or consent forms. Sending reminders through secure email, text, or portal messages keeps them informed and reduces back-and-forth.
In LeadSquared, you can configure this flow by storing authorization dates in patient records, then creating automation rules around those fields. For example:
- If an authorization is set to expire in 30 days, trigger an email to the family and a task for the coordinator.
- If hours used are at 80% of the total authorized, notify the billing team and create a task to begin renewal.
- Track all communications in the patient timeline so nothing slips through.
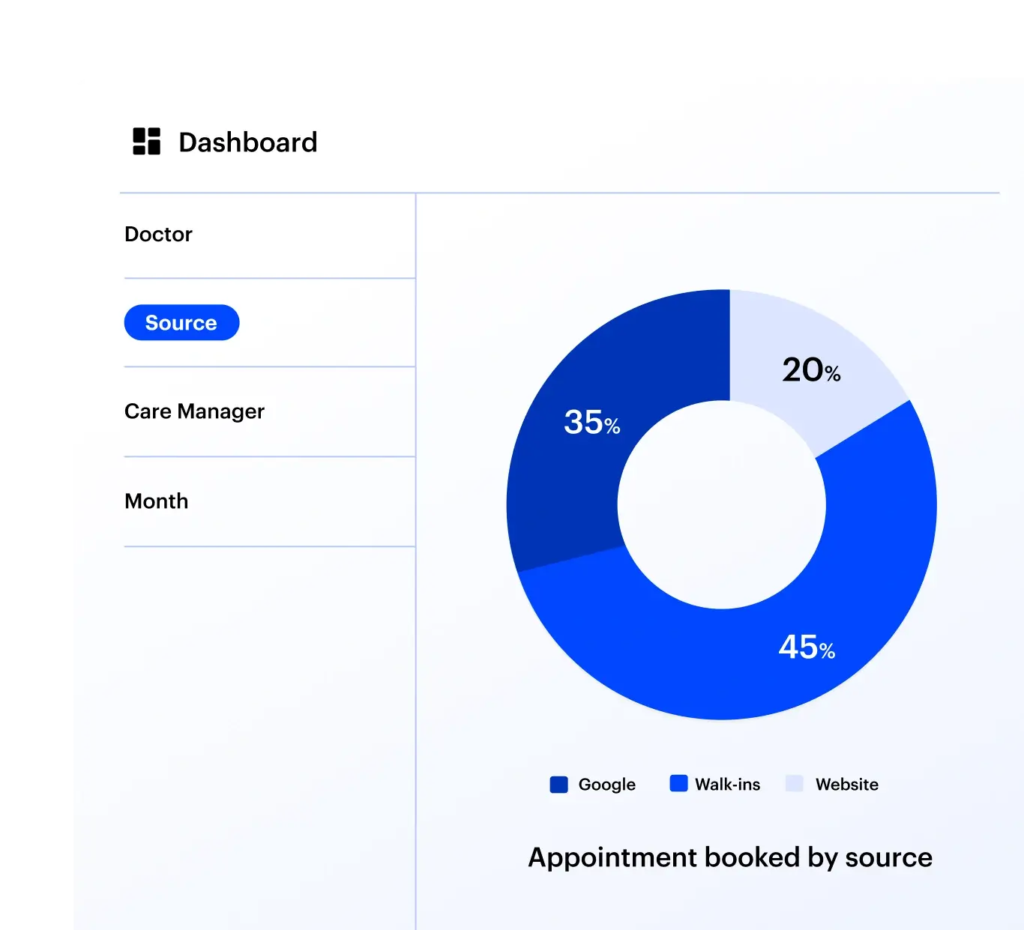
Dashboards can give leadership visibility into reauthorization activity, showing how many patients are approaching expiration, how many have already submitted requests, and where delays are happening.
By automating reauthorization reminders, clinics can reduce service interruptions, improve compliance with payer requirements, and ease the administrative burden on staff—while giving families confidence that their child’s therapy will continue without unnecessary breaks.













 Read the full story
Read the full story