Powering better
outcomes inEducationFinanceHealthcare
Loved by 1600+ organizations worldwide








Loved by 1600+ organizations worldwide








BEFORE

AFTER
Respond in seconds, with verified answers
BEFORE

AFTER
Automate key processes to reduce overload.

BEFORE

AFTER
Auto-schedule, remind, and confirm

BEFORE

AFTER
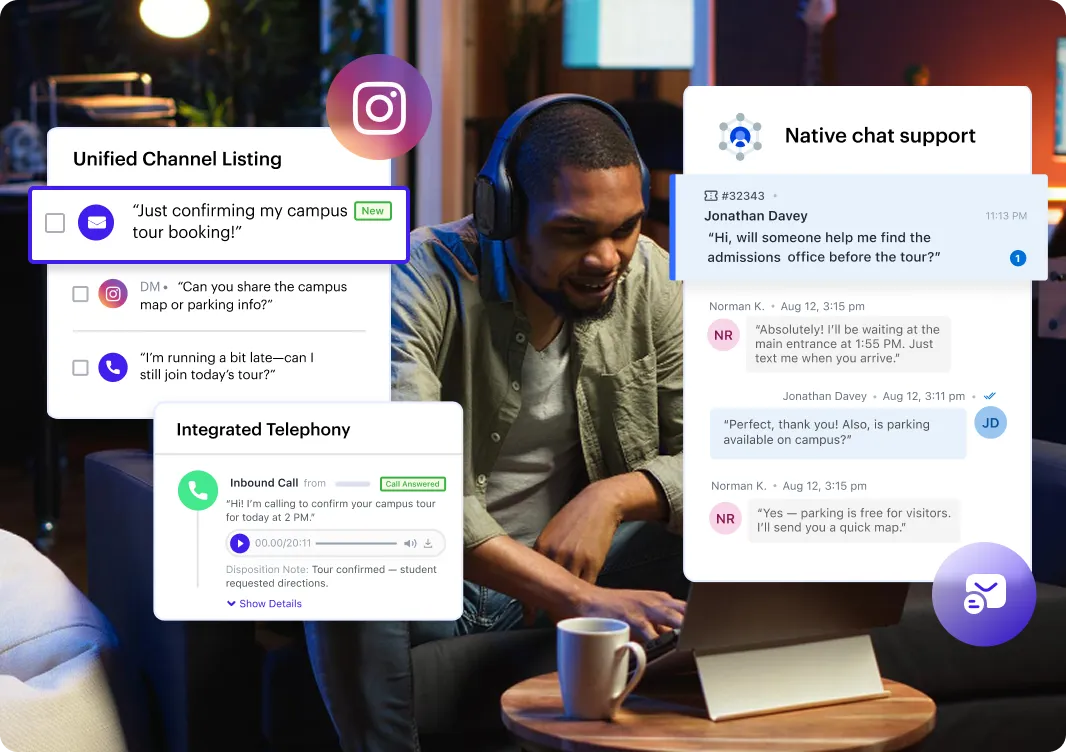
One surface for chat, SMS, email, and calls
BEFORE

AFTER
FERPA and HIPAA aligned controls baked in

Higher team capacity without
overwhelm
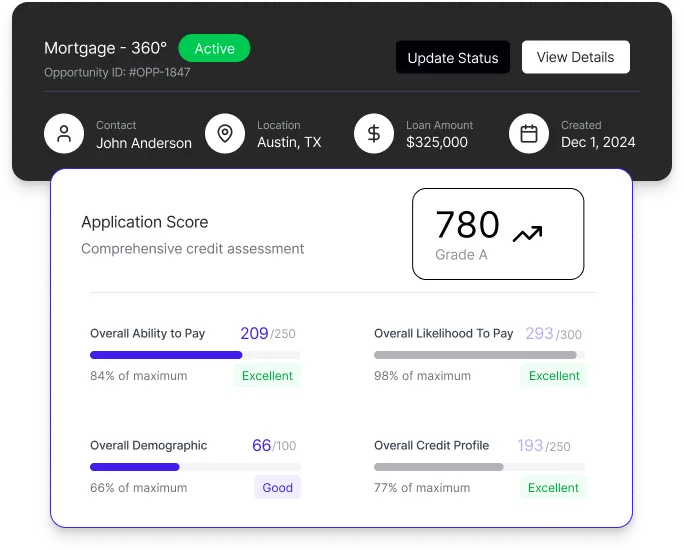
Higher referral conversions through automation
Faster lead response TAT with quicker, real-time engagement
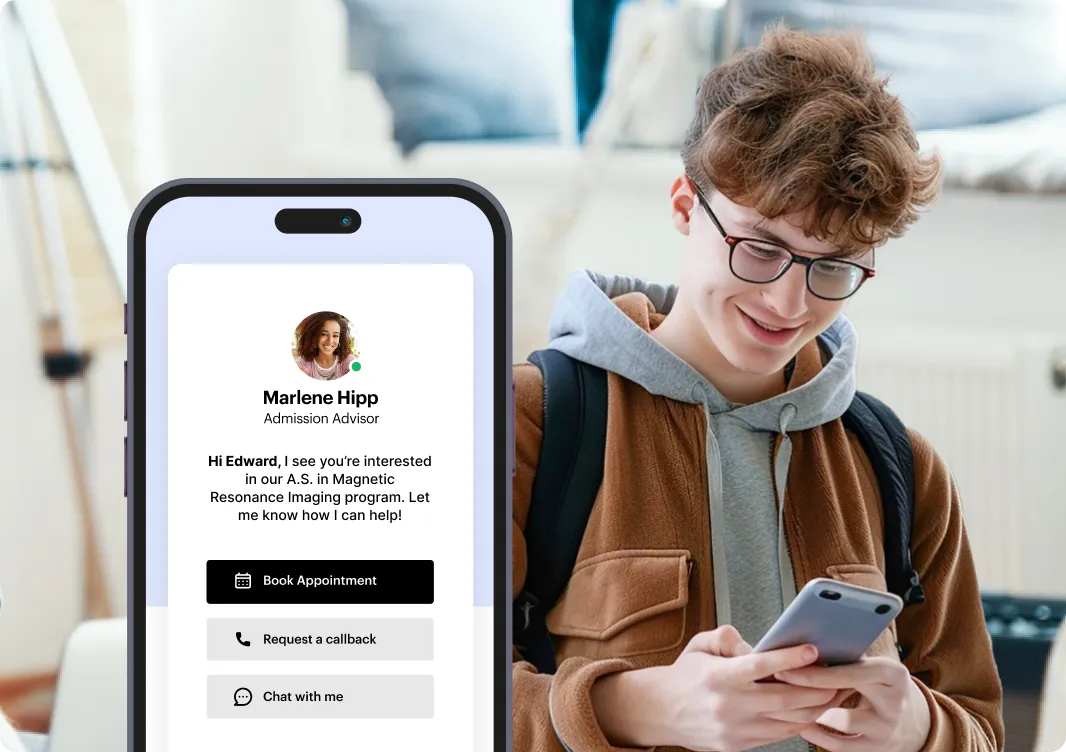
Intake and Admissions
Keep new contacts engaged and moving forward through the process, tracking them through every part of their journey.
Marketing Tools
Run all your campaigns—emails, text messages, and more—from one central hub. Use advanced segmentation to deliver the right message to the right people, every time.
Automation
Built-in automation streamlines staff workflows while delivering personalized outreach that fuels growth.
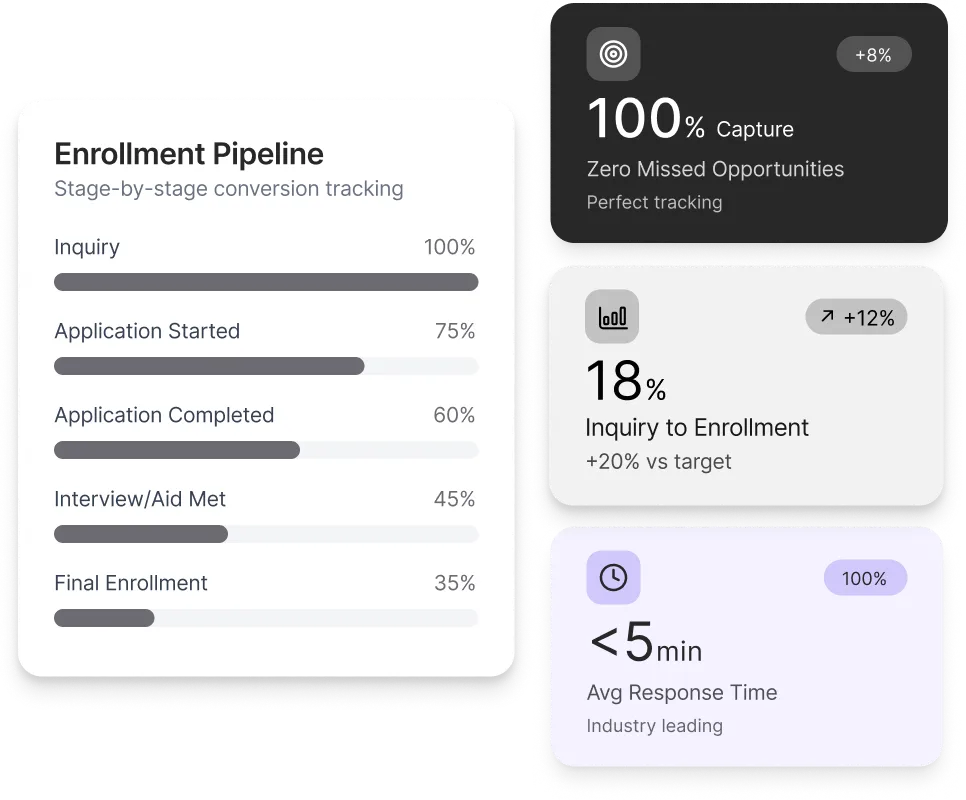
Analytics
Pull data from all your tools into a single source of truth. Turn it into insights with ready-made reports or build custom ones tailored to your needs.
Administration
Hit the ground running with an interface that’s easy for anyone to pick up and use, ensuring teams stay fast and responsive from day one.
Manage everything from one place—with the flexibility to keep some of your tools if you want, or replace them with ours as needed.
Industry-specific capabilities designed for real-world complexity.
Connect your SIS/EHR/LMS, scheduling, and analytics tools in minutes.









We specialize in streamlining workflows and boosting engagement.

LeadSquared’s implementation has transformed our operations completely, surpassing all other platforms we’ve used at Tandem.”

The LeadSquared solution enabled us to nearly double our referral coordinator productivity.


The system is so easy to learn and allows our admissions team to focus on supporting the student experience.


Since moving to LeadSquared, the average response time has improved to just 2.7 minutes. This has accelerated our contact rate and increased conversions.

How does “governed AI” differ from basic AI features?
Governed AI ensures every AI action follows your organization’s rules, permissions, compliance needs, and data boundaries. Unlike basic AI, which generates insights without oversight, governed AI is controlled, auditable, role-based, and aligned with your internal policies—so teams get the benefits of AI without security or compliance risks.
Is LeadSquared FERPA and HIPAA aligned?
Yes. LeadSquared follows strict data-handling, access-control, and security practices aligned with FERPA and HIPAA requirements. This includes encrypted data storage, role-based access, audit trails, and secure sharing protocols to support institutions that manage sensitive student or patient information.
How quickly can we go live?
Most teams go live within a few weeks, depending on complexity, data migration, and integrations. LeadSquared provides guided onboarding, best-practice templates, and prebuilt workflows to help you launch faster and start seeing value immediately.
Do we need to replace our existing tools?
Not at all. LeadSquared integrates with your existing systems—SIS/CRM, EMR, telephony, payment gateways, LMS, marketing tools, and more. You can keep using the tools you prefer and simply connect them to create a unified workflow.
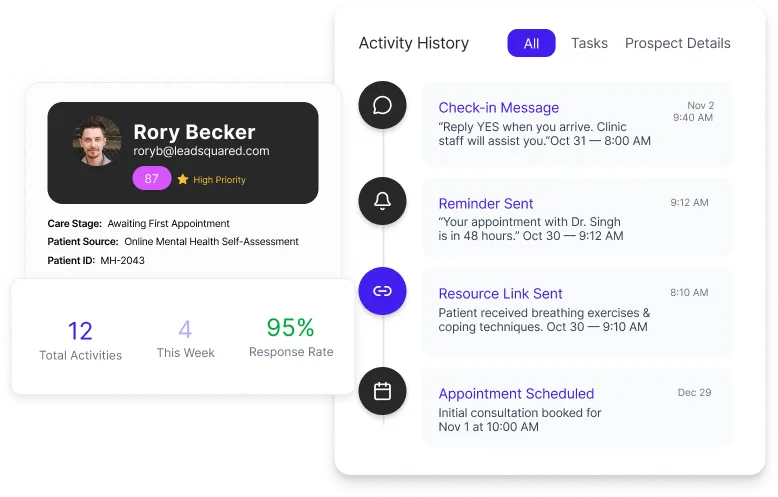
What data does Smart Answers use?
Smart Answers uses the data already available in your LeadSquared account—your records, activity history, workflows, communication logs, and configured fields. It does not use external or customer-identifiable data outside your controlled environment.
Can we customize workflows for our teams?
Yes. Every workflow—whether for admissions, sales, service, patient intake, or routing—can be customized without code. You can tailor processes by team, department, location, or business rule, ensuring each group works the way they need to.
We help you automate, personalize, and track every journey so your teams
stay informed and nobody falls through the cracks.