- Home
- Learn
- Healthcare
- How To Manage An ABA Waitlist: A Comprehensive Guide For Healthcare Providers
HEALTHCARE
How To Manage An ABA Waitlist: A Comprehensive Guide For Healthcare Providers
Contents
One of the most sought-after treatments for children with autism spectrum disorder (ASD) and other developmental conditions is Applied Behavior Analysis (ABA) therapy. As demand continues to rise, healthcare professionals in the US are dealing with more complicated ABA therapy waitlists. Effectively managing an ABA waitlist involves more than just structure; it includes upholding trust, fostering optimism, and making sure that families get the assistance they require.
Organizational success, employee morale, and family satisfaction all benefit from an investment in efficient waitlist management. Healthcare organizations will be in a better position to serve their patients and fulfill their objectives of improving outcomes for children with developmental impairments, including autism, if they give priority to this area of their operations.
ABA waitlist management is much more complicated than first-come, first-served scheduling. Clinical priority assessment, family communication, resource allocation, and strategic planning must all be carefully balanced. For healthcare organizations, a well-managed ABA waitlist can be the difference between a thriving practice that creates enduring relationships with the communities they serve and disgruntled families looking for services elsewhere.
With 1 in every 31 children diagnosed with autism spectrum disorder, according to the Centers for Disease Control, the demand for ABA therapy has surged in recent years. As awareness of its benefits grows alongside rising diagnosis rates, the need for ABA services now far exceeds the available resources.
Waitlists for ABA therapy have become widespread in the US, with some families having to wait months or even years before receiving assistance. Given that early intervention is essential to optimizing therapeutic outcomes, this delay can be very difficult for families. Families and healthcare professionals often experience frustration and anxiety due to long wait times and unpredictable scheduling.
Healthcare organizations need to understand that keeping an ABA waitlist under control is more than just an administrative chore; it’s an essential part of patient care that has a direct impact on clinical results, family satisfaction, and the long-term viability of the practice. Negative reviews, lost income, and—most importantly—delayed care for kids who need urgent attention can all be consequences of a poorly managed waitlist.
A thorough strategy framework that takes into account several aspects of the problem is necessary for efficient ABA waitlist management. Intake procedures, priority guidelines, communication tactics, resource allocation, and mechanisms for ongoing improvement should all be included in this framework.
Understanding your current capacity and anticipated expansion is the first step in building a good waitlist management system. To set reasonable deadlines for new patient intake, healthcare practitioners must assess their availability of therapists, treatment rooms, scheduling flexibility, and administrative support. Because capacity can be greatly impacted by factors like staff turnover, facility modifications, and service expansions, this assessment should be ongoing.
The foundation of ethical and efficient waitlist management is made up of prioritization procedures. These procedures ought to take into account variables like the child’s age, the degree of demand, the family’s situation, and insurance coverage. These procedures must take resource optimization and clinical best practices into consideration while preserving equity and openness.
The intake procedure establishes the tone for the whole family experience and acts as the entry point to your ABA waitlist. An effective patient intake process should be comprehensive but efficient, collecting all relevant data while easing the strain on already overburdened families.
Start by developing standardized intake forms that include clinical history, prior therapy experiences, insurance information, family preferences, and important demographic data. To accommodate varying family preferences and degrees of technical comfort, these forms should be available via a variety of channels, including online portals, phone interviews, and in-person meetings.
Preliminary assessments are essential during the intake process to determine whether ABA therapy is suitable for each child. The child’s present functioning level, specific behavioral issues, family objectives, and preparedness for intense intervention should all be assessed. Early detection of these cases helps avoid needless waitlist congestion, as not all children referred for ABA therapy would be suitable candidates.
Establishing documentation standards is necessary to guarantee that all pertinent data is reliably recorded and readily available for use in placement decisions. In addition to clinical data, this paperwork should cover scheduling restrictions, family preferences, and necessary special accommodations.
One of the hardest things about managing an ABA waitlist is coming up with a transparent and equitable priority mechanism. While upholding clinical best practices and ethical norms, the system must strike a balance between several conflicting factors.
Most systems are built on age-based prioritizing since research continuously shows that earlier intervention produces better results. Age, however, cannot be the only deciding criterion because older kids could have more serious requirements or might have been waiting longer for assistance.
When assessing the severity of needs, behavioral issues, developmental delays, and the effect on family functioning, it must all be carefully taken into account. Qualified professionals who can impartially analyze each child’s presentation and choose the right level of assistance should assess this.
Prioritization decisions should take into account family conditions, such as caregiver availability, sibling requirements, and social support networks, as these can have a substantial impact on therapeutic outcomes. Families with strong support networks could wait a little while longer for services, while those with weaker support networks might require more attention.
Though contentious at times, geographic location and insurance coverage frequently have useful functions in setting priorities. Geographical factors can affect the effectiveness of therapy delivery and family compliance, while families with low insurance coverage could require more time to obtain funding.
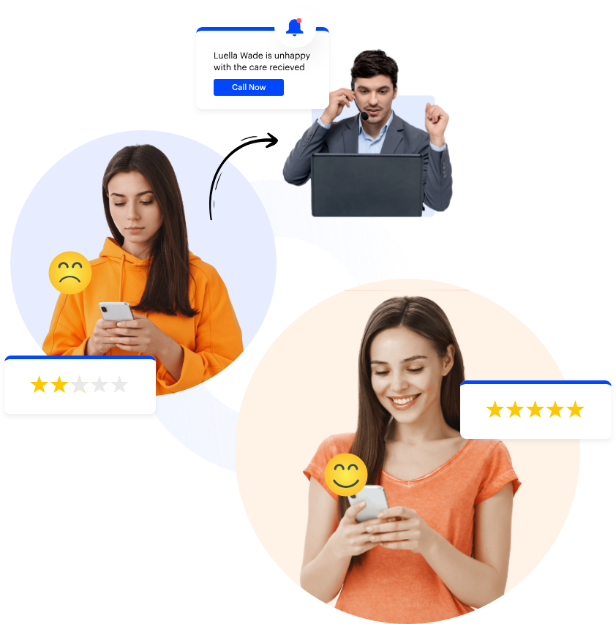
The key to managing an ABA waitlist successfully is effective communication. Clear, regular communication can help ease some of the tension and anxiety that families on your waitlist often experience while also fostering trust in your organization.
Families should be given clear information on what to expect throughout the waiting period, as well as realistic expectations regarding wait times and the priority process. While giving as much detailed information as possible regarding the procedure and schedule, this communication should be open and honest about any uncertainties.
Maintaining family involvement and confidence during the waiting period requires regular updates. Any modifications to the anticipated wait durations, the status of the waitlist progression, and any new information or supporting paperwork that could be required should all be included in these updates. Typical wait times and family preferences should be taken into consideration when deciding how frequently these updates should be sent.
Through customized, HIPAA-compliant email and text workflows, LeadSquared’s Healthcare CRM can automate these updates, keeping families informed without increasing the administrative burden on your staff.
In addition to making families feel supported during the waiting period, offering them educational materials and support may enhance the results of therapy after services start. These resources could include behavior management techniques, community services, support groups, and information about autism and ABA therapy.
Establishing a variety of contact channels guarantees that families can get in touch with your organization with any queries or worries they may have. Phone assistance, email correspondence, client portals, and maybe text messaging for urgent updates should all be part of these channels.
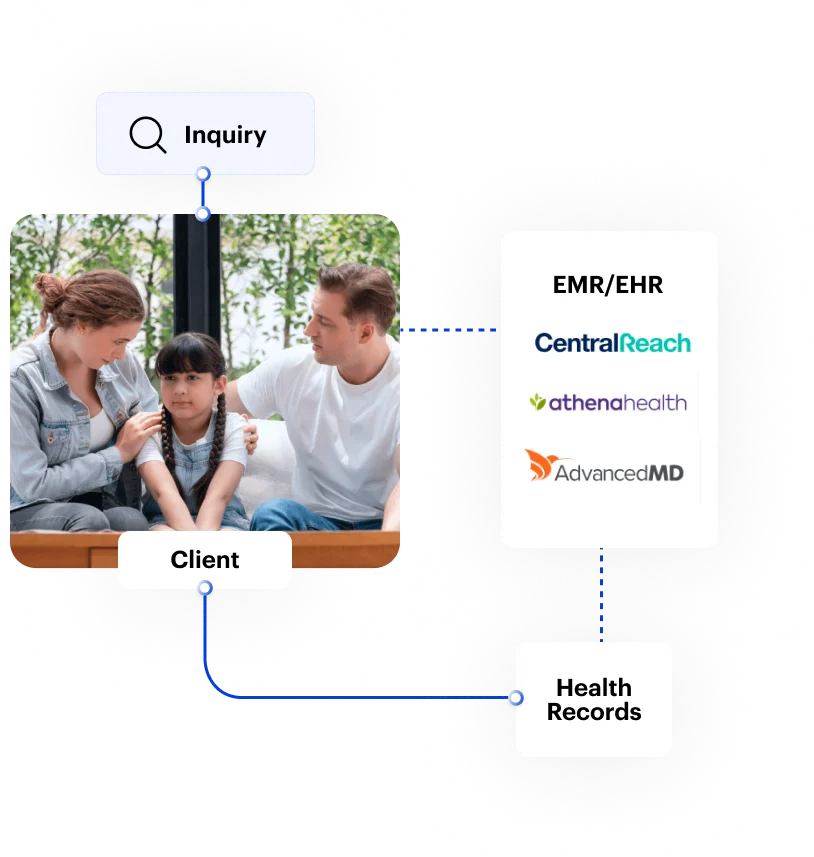
Sophisticated technology platforms that can manage the intricacies of resource planning, communication, and prioritization are necessary for modern ABA waitlist management. Customer relationship management (CRM) systems tailored to the healthcare industry have become effective instruments for handling these intricate processes.
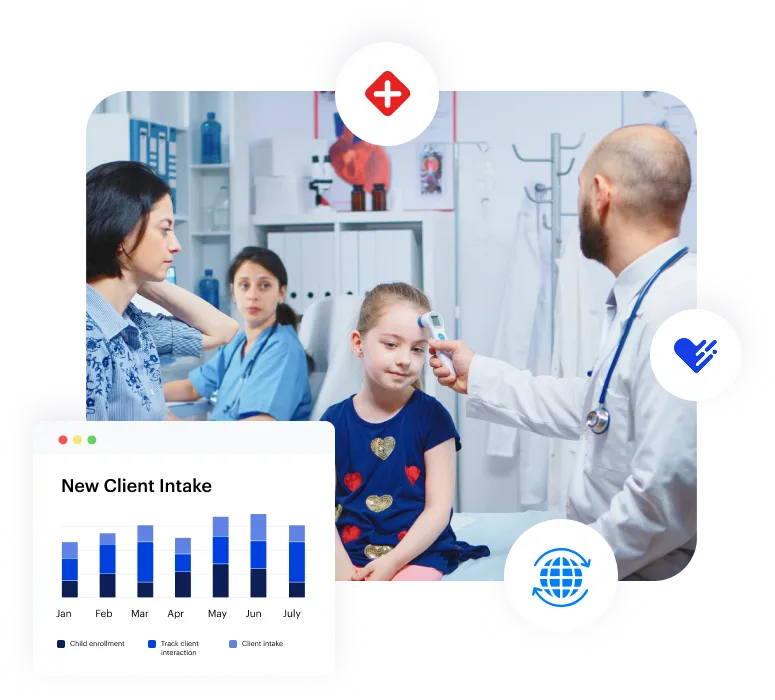
Platforms like LeadSquared for healthcare were created especially to handle the particular difficulties that healthcare organizations encounter when handling intricate patient journeys. Many waitlist management tasks can be automated by a strong CRM system, with the flexibility to deal with special circumstances. These systems can monitor wait times, control communication sequences, keep tabs on family information, and produce reports that support capacity planning and performance evaluation.
Solutions that comprehend the complexity of healthcare patient journeys are necessary for healthcare organizations managing ABA waitlists. From the first inquiry until the provision of services, LeadSquared’s Healthcare CRM platform offers specialized solutions for handling multi-step patient procedures. The complex prioritization algorithms required for ABA waitlist management may be handled by the platform’s automated workflow features, all the while preserving the human touch that families anticipate during trying waiting times.
LeadSquared provides specialized features like automated patient journey mapping, HIPAA-compliant communication tools, and real-time reporting dashboards that give insight into waitlist performance for healthcare organizations in the US, managing complicated ABA therapy waitlists. A cohesive ecosystem for managing the complete patient experience is created via the platform’s integration features, which enable a smooth connection with current scheduling systems, electronic health records, and billing platforms.
Healthcare companies may track waitlist performance, spot bottlenecks, and make data-driven choices on resource allocation and process enhancements thanks to reporting and analytics tools. Securing more funding for program expansion and proving value to stakeholders can both be greatly backed by these insights.
Planning resources and managing capacity are crucial for efficient ABA waitlist management. The necessity to maintain sustainable operations and high-quality services must be balanced with the goal of serving as many families as feasible.
Strategies for attracting and keeping therapists are essential for controlling waitlist length and guaranteeing service quality. Competitive pay packages, chances for professional growth, realistic caseload expectations, and encouraging work cultures that lower burnout and attrition are all examples of this.
The unique requirements of ABA therapy, such as suitable space for individual and group sessions, sensory considerations, and safety standards, must be taken into account while designing a facility. Long-term demand forecasts and a thorough examination of waitlist trends should serve as the foundation for any expansion decisions.
Without using more resources, scheduling optimization can have a big influence on capacity. This could entail extending business hours, providing weekend sessions, using telemedicine options where suitable, and putting in place flexible scheduling plans that maximize therapist efficiency while accommodating family demands.
Opportunities for collaboration with other medical facilities, educational institutions, and neighborhood associations can aid in increasing capacity and easing the strain on waitlists. These collaborations could involve cooperative service delivery approaches, referral networks, or pooled resources.
It takes strong quality assurance procedures and a dedication to ongoing development to maintain high-quality services while handling waitlists. Healthcare institutions must make sure that the standard of treatment given to families is not jeopardized by the drive to shorten waitlists.
The delivery of treatment services and waitlist management procedures should both be evaluated by routine quality audits. Effective communication, fair prioritization, wait time accuracy, and family satisfaction should all be assessed throughout these audits.
Family feedback systems can point out areas for improvement and offer insightful information about the waitlist experience. It is important to gather, examine, and apply this input in a methodical manner to enhance the process.
Programs for staff development and training make sure that everyone on the team is aware of their responsibilities in waitlist management and has the abilities necessary to give waiting families outstanding customer care.
Organizations can monitor progress and spot trends with the aid of performance metrics and key performance indicators (KPIs). Average wait durations, family satisfaction ratings, waitlist-to-active therapy conversion rates, and staff productivity indicators are a few examples of these metrics.
ABA waitlist management is subject to a number of industry norms and healthcare laws. Healthcare institutions need to make sure that their waitlist procedures respect patient confidentiality, keep accurate records, and adhere to insurance regulations.
When handling patient data during the waiting procedure, HIPAA compliance is crucial. This entails managing communications containing protected health information carefully, implementing suitable access restrictions, and securely storing family information.
Waitlist management may be impacted by insurance rules, especially those pertaining to service delivery standards, documentation requirements, and authorization timelines. Organizations need to make sure that their waitlist procedures facilitate prompt insurance processing and don’t obstruct coverage.
State and federal regulations may impose specific requirements on ABA services, such as staff credentials, supervision ratios, and service documentation. To ensure compliance, waitlist management processes should be designed with these guidelines in mind from the outset.
Families may find the waiting time especially difficult, and healthcare institutions have a chance to offer helpful assistance that can enhance results and fortify bonds.
In addition to helping families better understand what to anticipate, educational materials regarding autism, ABA therapy, and behavioral methods may also enhance therapy results after services start. These materials ought to be easily available, suitable for different cultural contexts, and updated frequently to take advantage of the latest best practices.
Families can receive extra assistance throughout the waiting period by connecting with local services and support organizations. Information about nearby support groups, respite care services, educational advocates, and other medical professionals may be included.
Families can prepare for the start of ABA therapy by engaging in preparation exercises. Baseline evaluations, goal-setting activities, setting up the home environment, and family education on fundamental behavioral techniques may all fall under this category.
Families that are facing serious difficulties throughout the waiting period should have access to crisis support. In extreme cases, this could entail expedited placement, resource referrals, or consultancy services.
Careful evaluation of ROI and success is necessary for efficient ABA waitlist management. Healthcare institutions need to know whether their waitlist management initiatives are benefiting workers, families, and the organization as a whole.
Measures of family satisfaction shed light on the waitlist experience and also point out areas that need work. When accessible, these measurements ought to be compared to industry norms and gathered in a methodical manner.
Organizations can assess the effectiveness of their waitlist management procedures by using operational efficiency metrics. Metrics pertaining to employee productivity, communication efficacy, and process cycle times may be included.
A financial impact study ought to weigh the advantages and disadvantages of waitlist management initiatives. This covers both the direct expenses of staff time and technology as well as the indirect advantages, such as favorable word-of-mouth recommendations.
By demonstrating better therapy outcomes for families that had great waitlist experiences, clinical outcomes tracking can assist in proving the importance of efficient queue management.
A number of developments are expected to influence how healthcare institutions handle these issues in the upcoming years as the field of ABA therapy and waitlist management continues to change.
Integration of telehealth has sped up significantly and could open up new possibilities for waitlist management and service delivery. To serve more families with the resources already available, this may involve hybrid service delivery methods, remote parent education, and virtual evaluations.
Technologies related to artificial intelligence and machine learning could offer new resources for resource optimization, demand forecasting, and queue prioritization. These technologies have the potential to assist organizations in making better judgments regarding family placement and capacity planning.
Value-based care models have the ability to alter waitilist management tactics by altering the way ABA services are provided and paid for. To comply with outcome-based payment models and quality indicators, organizations might need to modify their strategies.
Waitlist management procedures will probably be impacted by a greater emphasis on family-centered care and cultural competency, requiring that organizations be more sensitive to the various requirements and preferences of families.
Effective ABA waitlist management necessitates a multifaceted strategy that strikes a balance between clinician goals, family requirements, organizational sustainability, and financial limitations. Implementing reliable systems, technologies, and procedures while retaining the adaptability required to handle special scenarios and evolving conditions is essential for success.
As demand for ABA therapy continues to grow, organizations that master the art and science of waitlist management will gain a significant competitive advantage. By taking a structured approach, leveraging right technology, and committing to continuous improvement, healthcare providers can turn the difficulty of managing an ABA waitlist into an opportunity to enhance care delivery, and build stronger relationships with families.
The future of ABA therapy depends on how well organizations manage the process from initial contact to service delivery, in addition to the quality of services provided. By implementing the strategies and recommendations we just discussed, healthcare practitioners can ensure that their waitlist management practices align with their overall objective of providing exceptional care to children and families in need.
LeadSquared’s Healthcare CRM system offers the necessary tools required to succeed in this demanding climate for healthcare institutions prepared to advance their ABA waitlist management. It helps healthcare companies turn their waitlist management from a cause of stress into a competitive advantage with features tailored for healthcare patient journey management, automated communication workflows, and extensive reporting tools.
Want to know more?
Managing high demand, ensuring timely follow-ups, tracking patient status, and preventing drop-offs are key challenges. Many providers struggle with disorganized outreach and outdated manual tracking methods, which delay care and lead to lost opportunities.
A HIPAA-compliant CRM like LeadSquared helps streamline waitlist workflows, automate communication, and reduce administrative friction—so patients don’t fall through the cracks.
Consistent, informative communication is critical. Families want to know they haven’t been forgotten, and updates—even small ones—help maintain trust and reduce no-show risk when a spot opens.
LeadSquared allows providers to automate personalized emails, text messages, and status updates, ensuring families remain informed and supported throughout their wait.
Many ABA providers use spreadsheets or EMRs that lack visibility into referral urgency, insurance status, and intake readiness—making fair prioritization difficult.
With LeadSquared’s customizable intake forms and intelligent lead scoring, you can prioritize families based on clinical urgency, location, payer type, and more—all in one centralized dashboard.
Yes! LeadSquared offers a HIPAA-compliant CRM tailored for healthcare, helping ABA practices track leads, automate waitlist workflows, and stay audit-ready—all while protecting patient data.
Scaling up often leads to burnout if not managed properly. Efficient intake, routing, and scheduling systems help teams handle more cases without increasing manual work.
Traditional CRMs often lack the healthcare-specific compliance and features ABA providers needs. You can use a CRM like LeadSquared that is specially built for healthcare; by automating repetitive tasks like documentation requests, follow-up scheduling, and appointment reminders, it frees your team to focus on high-value interactions.
To keep staffing balanced while managing waitlists, it helps to have a clear picture of both therapist availability and patient demand across all locations. Most ABA practice management software or CRMs allow you to track staff schedules, caseloads, and waitlists in one place.
In tools like LeadSquared, for example, you can view therapist assignments and caseloads across multiple sites. This makes it easier to see which locations are approaching capacity and which therapists have openings. You can also set rules around staffing ratios so the system can flag when adding a patient would exceed the recommended therapist-to-patient ratio.
Waitlist management features help organize incoming patients based on factors like urgency, age, or therapy type. Some systems even let you automatically prioritize families, which reduces the need for manual follow-ups.
Reporting across locations provides additional insight. You can identify trends, such as which clinics have the longest waitlists or which therapists are consistently at capacity. This data helps you make staffing decisions and allocate resources effectively.
By centralizing staffing and waitlist information, your clinic can maintain proper ratios and make sure families are served promptly regardless of which location they visit.
Managing intake across multiple locations requires visibility and coordination. Each team may handle inquiries differently, so centralizing information is key. Most ABA practice management software or CRMs allow you to track all intake activity in one system, making it easier to manage teams across sites.
In tools like LeadSquared, you can assign leads to specific locations or intake teams automatically based on factors like ZIP code, service type, or referral source. This ensures families are connected to the right team without manual routing. Teams can access the same platform to update intake status, schedule appointments, and track follow-ups, keeping everyone aligned.
You can also set up workflows and task assignments per location. For example, if one office has higher demand, the system can automatically flag pending inquiries or escalate follow-ups, ensuring no lead gets missed. Conditional rules can handle special cases, such as urgent referrals or age-specific therapy needs.
Reporting and dashboards provide an overview of activity across all sites. You can see which teams are handling the most inquiries, identify bottlenecks, and track conversion rates by location. This data makes it easier to balance workloads, plan staffing, and optimize intake processes across the organization.
Start by building a small, maintainable library. Include plain-language guides on what ABA is, how assessments work, and how to prepare for the first visit. Add simple home activities by age band, short videos that show what sessions look like, and practical checklists for documents, insurance, and scheduling. You can tag each item by age, program type, location relevance, and language so it is easy to route later.
Capture a few fields at intake to personalize. Age, preferred location, language, and program interest are usually enough. Make these mandatory so every waitlisted family can be placed in the right segment. If you collect communication preferences (and you should), store them as well so you respect clients’ opt-ins and preferred channels.
Once the library and fields are ready, set up delivery of the content using a CRM or ABA practice management software like LeadSquared. Create segments that mirror real scenarios, such as toddlers awaiting initial assessment, school-age families waiting at a specific clinic, or families pending insurance review. Pair each segment with a short sequence that sends the most useful items first, then spaces follow-ups at sensible intervals. Use email for longer guides and videos. Use text messages for quick reminders and links to one-page tips.
Automation keeps this consistent without extra workload. When a family is added to a waitlist, enroll them in the correct sequence automatically. If their age band changes or they switch locations, move them to the right segment. When a spot opens, send next-step instructions and alert the coordinator. If a family has not engaged after a set period, create a task for a personal check-in.
Track engagement and use it to improve the library. Monitor opens, clicks, video views, and downloads by segment. Retire content that families do not use, and expand on topics that consistently help. Flag families who engage heavily so coordinators can prioritize them for outreach when slots become available.
In LeadSquared, this workflow is straightforward. You can store the intake fields that allow segmentation, maintain dynamic lists by age and location, and run automated journeys that deliver emails or texts with links to your guides and videos. The software also allows you to attach resources to records, log interactions, and create tasks when families engage or when they do not.
Dashboards show engagement by segment so staff can spot who needs a call. If you also use the chatbot, it can share links after hours, collect basic questions, and route anything complex to the right person the next morning.
Managing waitlists in ABA often comes down to two challenges: prioritizing by geography and making sure age or service eligibility is factored in. The right tools let you segment families clearly, shorten wait times, and make scheduling decisions without juggling spreadsheets.
Location-based waitlist management
Start by capturing ZIP code, city, or clinic preference during intake. A healthcare CRM or ABA practice management system like LeadSquared can then help you tag each lead or patient record with their closest center. With that data in place, you can:
Maintain separate waitlists for each clinic location.
Use geo-filters or “distance to clinic” rules to assign families to the right list automatically.
Route new inquiries directly to the right coordinator based on coverage area. This prevents a single global waitlist from getting messy and ensures families are only considered where service is available.
Age and service-fit filtering
Age is another key field to capture up front. Many ABA programs have eligibility windows (for example, early intervention vs. school-age support). By making age a required intake field, you can:
Segment waitlists into buckets (e.g., 2–5 years, 6–12 years, teens).
Filter out children who are outside your service range, so your team doesn’t waste time on families you cannot serve.
Flag time-sensitive cases, like toddlers aging out of early intervention, so they can be prioritized before losing eligibility.
Automation to keep lists accurate
With automation in place, waitlist management becomes easier:
When a spot opens at a location, the system can pull the next eligible patient from the list.
Families approaching an age threshold can be flagged for re-evaluation or fast-tracking.
Coordinators can receive reminders to check in with families who have been waiting beyond a set timeframe.
Reporting and forecasting
Dashboards feature in ABA practice management software like LeadSquared can show how many children are waiting per location, average wait times, and age distribution. This helps leaders decide whether to shift staff, open new availability, or adjust outreach strategies.
LeadSquared can manage this workflow by using custom fields like Location and Age on each patient record. Automations can route families to the right intake queue, trigger alerts when criteria are met, and maintain segmented waitlists without spreadsheets. Coordinators can then pull filtered views (such as “All patients under age 5 waiting at Clinic A”) and take action quickly.
Over time, reports show where demand is highest, so staffing and scheduling decisions can be made based on data.