- Home
- Learn
- Healthcare
- How to Automate Patient Intake Forms in Healthcare
HEALTHCARE
How to Automate Patient Intake Forms in Healthcare
Contents
Clipboards, pens, crowded waiting rooms…
For many clinics and hospitals, the patient intake process is still stuck in the past. Paperwork flows in from every direction, sometimes incomplete, often illegible, and it eats into valuable staff time and delays patient care.
But it doesn’t have to be this way.
Healthcare is rapidly shifting toward smarter, more connected systems. And automating intake forms is one of the easiest yet impactful upgrades healthcare providers can make in this era of technology. Done right, it frees up your staff, cuts down on manual errors, and gives patients a smoother start to their care experience.
Mind you, this is not just about digitizing a PDF and calling it a day. True automation means the forms are not just online, but instead they’re integrated and automated. They work in the background, triggered by events like appointment bookings or referrals, with no extra clicks or calls required.
In this article, we break down exactly how to automate patient intake forms. We dive into what tools you would need, what pitfalls to avoid, and why a CRM like LeadSquared makes the process way smoother for both staff and patients.
Let’s get into it.
If you’ve ever walked into a clinic and been handed a stack of forms, asking everything from your name and date of birth to what surgeries you had 10 years ago, you’ve seen patient intake forms in action.
They’re the first point of contact between the patient and the healthcare system. The info they collect sets the tone (and accuracy) for everything that comes next: diagnosis, treatment, billing, compliance.
Here’s what they typically include:
These forms are important. But when they’re manual, they’re also a pain for patients and staff. The problems being they can get lost, misread, don’t always show up where they should and so on.
This is where healthcare workflow automation helps.
Instead of waiting for patients to fill these out with a pen in a waiting room, you can:
The result being faster check-ins, cleaner records and less chaos at the front desk.
Next up: let’s walk through how you actually set this up in your practice.
Let’s say you’re ready to ditch the clipboard for good, but not sure where to start. Here’s a simple, step-by-step guide to help you go from manual mess to automated intake.
You can’t automate with static PDFs or scattered form builders. What you need is a system that:
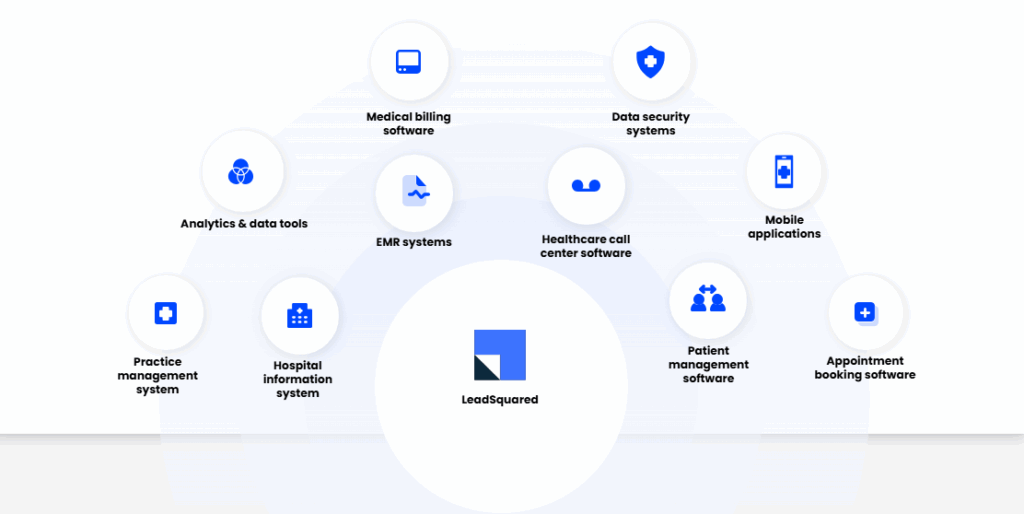
That’s where a healthcare CRM like LeadSquared comes in. It doesn’t merely handle forms, but instead connects them to the full patient journey, from the first call to post-visit follow-ups to collect and organize data efficiently.
Your forms should be intelligent and comprehensive.
Look for features like:
With the right automation in place, forms can be sent:
Each trigger makes sure the form goes out at the right moment, based on where the patient is in their journey.
In this day, it’s safe to assume most patients will complete their forms on a phone, instead of a desktop. So, test every form for:
If patients have to pinch-zoom their way through a form, they’re likely to abandon it, and that slows down your whole workflow.
The whole point of automation is to cut out the middle steps. So, the moment a patient hits “submit,” that data should:
Once the form is complete, your team should know instantly.
CRM dashboards and alerts help here to:
Some patients forget, others procrastinate. Either way, a simple automated reminder can make the difference between a fast check-in and a late start.
Set up follow-up messages like:
“Hi (Name), your intake form for tomorrow’s appointment is still pending. You can complete it here: (link)”
These reminders can go out as texts, emails, or via WhatsApp, or whatever your patients respond to best.
Not all “digital forms” are created equal.
Some tools let you build a basic online form and stop there. But true automation needs more than that. As we saw, it needs intelligence, integration, and the ability to work silently in the background.
Here’s what to look for when choosing a form automation solution:
Forms should adapt based on patient input instead of forcing everyone through the same 30 questions.
Look for tools that let you:
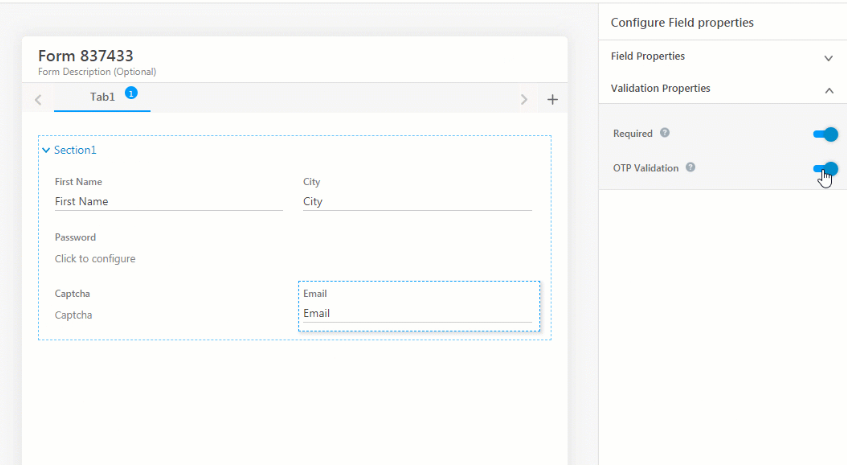
LeadSquared supports smart field logic and branching, so your intake forms stay short, relevant, and personalized. It also allows you to set up these forms natively or plug in your favorite form tools and sync the data straight into patient records.
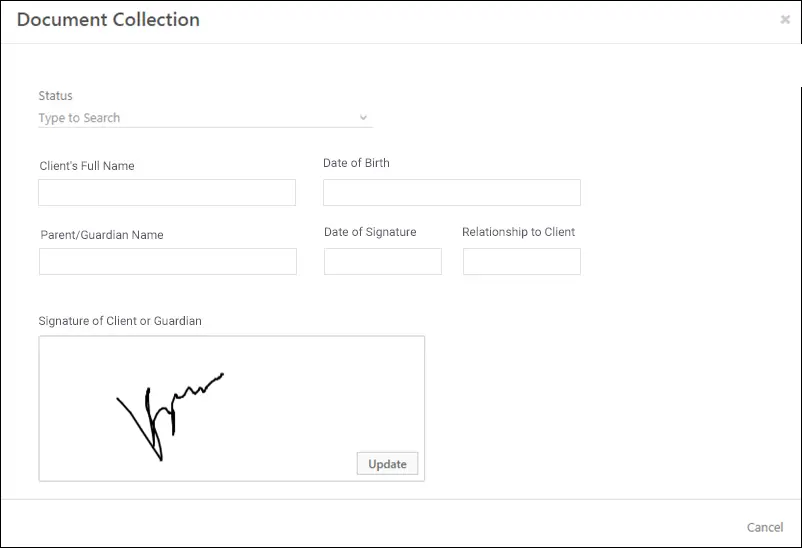
Patient forms often include sensitive authorizations and consent.
That means:
With LeadSquared, e-signatures are built into the workflow and meet compliance standards.
A form isn’t useful if it just sits in someone’s inbox.
It should:
LeadSquared’s intake forms sync with its CRM engine, and can integrate with other platforms via APIs, giving you a complete patient view, automatically.

Not every patient fills in their form the first time you ask.
Look for:
LeadSquared lets you set smart reminders that nudge patients until they complete their forms — and you can track exactly who’s done what.
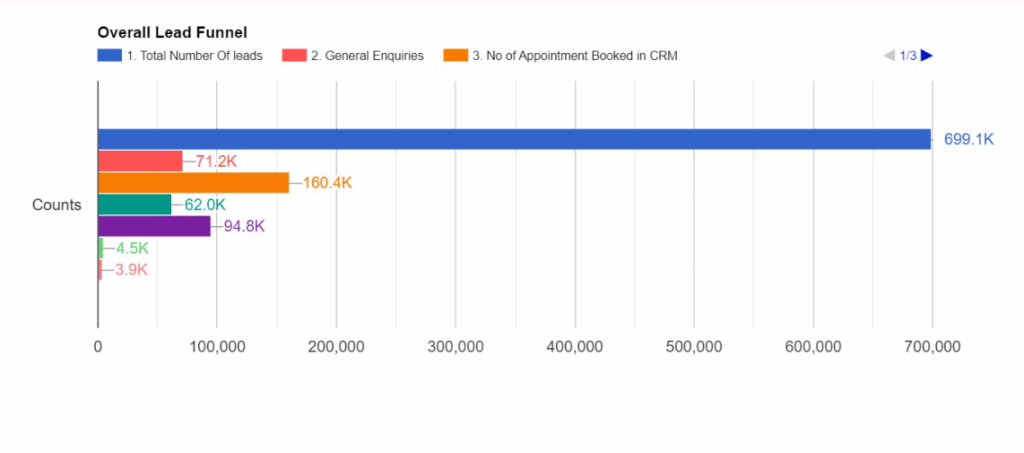
You can’t improve what you don’t measure.
A good system should tell you:
LeadSquared’s analytics and reporting feature offers dashboards that help you spot bottlenecks and optimize your forms to reduce drop-offs and increase appointment completion rates.
Your patients aren’t all the same, and your forms shouldn’t assume they are.
You’ll want:
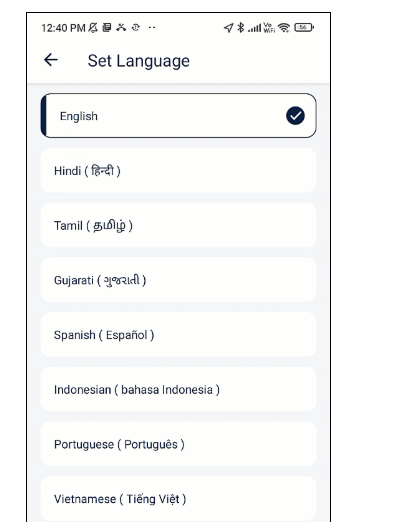
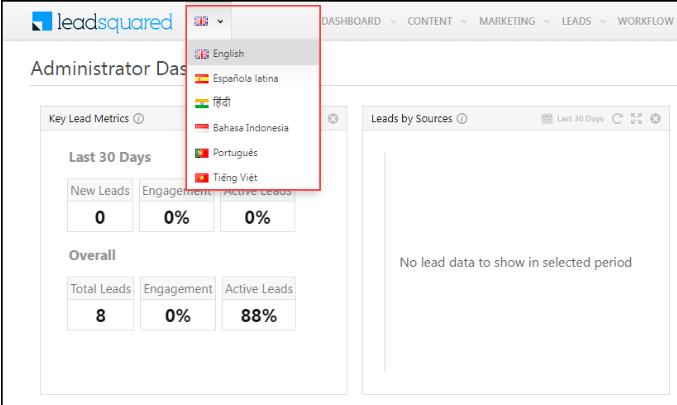
LeadSquared’s form templates are responsive and can be customized for different languages.

Automating your intake forms solves some of the most frustrating pain points in everyday clinic operations.
Here’s what gets better when you make the switch:
Manual data entry eats up hours, especially when front-desk staff are retyping handwritten forms or calling patients to fill in the blanks.
With automation:
It’s one of the fastest ways to free up your team’s time without having to hire more people.
Paper forms give space for a lot of problems to emerge, such as:
Automated forms help prevent all that with:
No one enjoys filling out a form in a crowded waiting room.
Automation lets patients:
When forms are automated, front-desk staff don’t have to:
Instead, they get a dashboard that shows who’s ready, who’s not, and what’s still pending.
With automated forms:
That means you’re not left scrambling during audits or legal reviews.
You can piece together a form builder here, a messaging tool there, and an EHR integration somewhere in the middle.
But a centralized system like LeadSquared’s healthcare CRM makes a real difference.
No more toggling between tools. With LeadSquared:
LeadSquared lets you create:
LeadSquared connects directly with your existing systems, so:
Your front-desk team gets instant insight into:
LeadSquared helps you send forms through channels patients actually use:
All communications are also tracked for you to know exactly what’s been seen or clicked or completed.
Even with the best tools, intake automation can fall flat if it’s not executed thoughtfully. These best practices can help you get the most out of your setup.
Not every visit needs a full medical history.
Tailor your forms based on:
The shorter the form, the more likely patients are to complete it.
If a patient has already filled out their basic info once, don’t make them do it again.
Smart systems like LeadSquared can:
Most patients will complete forms on their phones — likely while juggling a dozen other things.
So,make sure your forms are:
A form that breaks on mobile is a form that doesn’t get completed.
Tech works best when your staff are proficient in using it.
Ensure your team:
Sometimes, all it takes is tweaking a subject line or text copy to get more patients to respond.
Try running small experiments like:
Then watch what works best and optimize from there.
If you’re looking for a fast, meaningful win in patient experience and operations, automating your intake forms is it.
It reduces check-in chaos and saves hours of manual work. And most importantly, it creates a smoother experience for your patients.
Of course, forms are just one piece of the intake puzzle. If you’re ready to go deeper, we’ve put together a full guide that covers everything: workflows, tools, compliance, and real-world best practices. Explore our complete patient intake guide.
Or, if you’re ready to see how this works in action, book a demo of LeadSquared’s Patient Intake CRM and see how much simpler your day can get.
Customize by using conditional logic—show only relevant questions—and update forms regularly based on patient feedback. Branding and clarity help patients feel comfortable, and clear, easy-to-follow instructions (via email or text) make forms simpler to complete.
Yes! Some systems use OCR and AI to read scanned documents, extract key data and sync it into the system. This reduces manual entry and speeds up processing.
Key mistakes include:
Overloading forms with unnecessary questions
Neglecting mobile design
One-size-fits-all templates without personalization or logical flow.
Fix these with brevity, responsiveness, and branching logic that adapts based on patient needs.
Automated forms create secure, time-stamped digital records with audit trails—all encrypted and stored centrally. This minimizes risk of lost paperwork or inconsistent storage, making compliance (HIPAA, GDPR) far easier.
Not if done thoughtfully. Self-service check-in can actually enhance the experience, often faster than manual processes. Plus, you can still offer support options (concierge help, optional traditional check‑in) to maintain warmth and personal touch.
Yes! Tools that include OCR (optical character recognition) can scan paper documents and extract key info into digital records. While handy for legacy forms, fully digital intake (built via form tools) offers cleaner data and fewer errors.
Help patients embrace change with clear, friendly guides and reminders. A quick text or email before their first form explaining why it matters—and how to fill it—can boost completion rates. Adding a short instructional video or printable sheet can also ease tech anxiety.
Absolutely, especially in diverse patient communities. Offering intake forms in multiple languages increases clarity and trust, and helps reduce errors or drop-offs due to confusion. Make sure your form tool supports easy translation and mobile display.
Watch metrics like:
Form completion rate (how many fully submitted)
Average fill time
Drop-off points on fields
Check-in time vs. pre-automation
These insights help you identify friction and iterate intelligently.
Yes. Digital, contact-free forms reduce shared surface usage in waiting areas, minimizing infection risk. That’s one of the reasons digital intakes became a standard part of safer clinic protocols, even after COVID-19.
Absolutely. Many clinics automate intake by sending forms directly via SMS or email after booking, before the patient even logs into a portal. This avoids portal delays while capturing key data early.
Clinics tend to gravitate toward healthcare-specific tools and CRMs that natively integrate with EHRs. A common pain point: general form tools may lack that deep EHR sync, making healthcare-dedicated platforms far more reliable.
HIPAA is non-negotiable, but enterprise-grade security also needs encryption, audit logs, and user access controls. Automated systems remove paperwork risk by storing signed, timestamped forms securely, giving you both compliance and visibility.
Automating patient communication in ABA begins by mapping out the key points of contact during the intake process. These usually include moments right after a referral comes in, an inquiry is made, or an appointment is scheduled. At each of these steps, families expect timely updates that explain what happens next.
With a CRM like LeadSquared, providers can set up workflows that automatically send emails or text messages based on specific triggers. For instance, when a new client inquiry is logged, the system can send a personalized welcome message. If a first session is booked, it can follow up with appointment details, intake forms, and preparation tips.
These messages are fully customizable and can include the client’s name, therapist assignment, session time, or clinic location. Workflows can also include time delays and follow-up conditions so communication stays relevant and well-paced.
Intake workflows in ABA therapy often include several steps: collecting basic client information, sending out consent forms, verifying insurance, and scheduling the first session. When these steps are handled manually, it can slow down onboarding and leave room for missed details.
Automation helps organize and streamline this process. For example, when a family submits an inquiry or signs up online, their information can be automatically logged into a centralized system. From there, forms can be shared digitally, and reminders can be scheduled to follow up if anything is left incomplete.
Each part of the workflow can be connected, so when one task is completed — such as submitting an intake form — it can trigger the next, like scheduling a consultation or assigning a provider. This keeps the process moving without the need for constant manual coordination.
The goal of automation isn’t just speed, but also consistency. It ensures that every family goes through the same essential steps, and that documentation is complete and accessible to the care team from the beginning.
Intake coordinators handle multiple repetitive tasks, from capturing new inquiries to scheduling appointments and following up with families. Automating these processes reduces manual work and keeps workflows consistent.
Most ABA practice management software or CRMs allow you to create automated workflows. In tools like LeadSquared, new inquiries from your website, email campaigns, or referral sources can automatically enter the system.
The software can then trigger follow-up emails, appointment reminders, or task assignments for the intake team without manual intervention. Forms can be set up with required fields and conditional logic, ensuring families provide all necessary information before submission. This minimizes back-and-forth communication and prevents incomplete intake records.
Automation can also handle task management. Coordinators can get real-time dashboards showing pending tasks, incomplete forms, or appointments needing confirmation. This ensures nothing falls through the cracks and helps prioritize follow-ups.
Reporting and analytics can be automated, too. The system can track how many leads convert, which referral sources are most effective, and where bottlenecks occur in the intake process. This gives your team actionable insights without manually compiling data.
You can use an ABA practice management software such as LeadSquared for tracking patient status and progress the intake funnel.
Start by defining the exact stages your clinic uses. Keep them specific and limited, so staff can understand them easily. For example, stages can include: Referral Received, Contacted, Documents Submitted, Insurance Verified, Assessment Scheduled, Authorization Approved, Treatment Start.
Capture the right data at each step. Along with the stage, store a small set of key fields you will report on, such as: referral date, contact date, documents received, payer name, auth expiry date, approved hours, assessment date, and treatment start date.
Next – automate status changes where possible. Link form submissions, document uploads, and verification results to the pipeline so the system updates the stage automatically. That reduces manual edits and keeps the pipeline current. For items that require human review, move the record to an exception queue.
Make ownership explicit. When a stage changes, assign the next task to the right person automatically. Use simple tasks and checklists so nothing is left ambiguous.
Set SLAs and alerts. Define how long a patient may sit in each stage before someone needs to act. When a record exceeds that time, notify the owner and create an escalation path to a manager.
Use dashboards available in the ABA practice management system. It shows how many patients are in each stage, average time per stage, and conversion rate from referral to treatment. You can also add filters for location, payer, and age to compare sites and spot where process changes are needed.
Set up a review process for exceptions. For example, if an insurance check fails, a document is missing, or the system isn’t confident about the data it pulled, those cases can go into a short review queue. Staff should be able to see the original file, the extracted details, and quickly approve or correct them with a single click.
Track the right KPIs and review them regularly. Measure time in each stage, stage-to-stage conversion rates, stalled case counts, and exception rates. Review these metrics weekly with intake leads and adjust workflows based on what the numbers show.
Some practical automations to implement now:
When an intake form is submitted, create the lead, and create a first-contact task.
When required documents are uploaded and pass QC, auto-advance the stage and notify billing.
If a record stays in Contacted for more than X days, send a reminder and escalate after Y days.
When authorization expires within 30 days, create a renewal task and notify the billing owner.
Make sure data quality is enforced at capture. Use required fields for the small set of items that drive routing, and use dropdowns for repeatable values like payer names. That reduces typos and avoids misclassification.
Healthcare CRM/ABA practice management software can also be used to keep stages, dates, documents, communications, and tasks on the same record. That enables reliable reporting and removes the need for spreadsheets.
You can also connect the system to insurance verification tools, document parsers, or scheduling systems so external events automatically update the intake funnel.