- Home
- Learn
- Healthcare
- Best Patient Management Software for Doctors
HEALTHCARE
Best Patient Management Software for Doctors
Contents
Doctors in the U.S. clock nearly 58 hours a week, but less than half that time is spent with patients, according to a 2024 AMA survey.
So where does the rest of their time go?
Mostly to paperwork and other administrative tasks that slow down care.
To tackle these challenges, practices increasingly rely on Patient Management Software (PMS) – a tool designed to simplify the usual admin responsibilities and keep the clinic running well.
In this article, we’ll explore the best PMS options out there for doctors in the U.S. We’ll, highlight features and value of each of these tools to help you find the right fit for your practice.
As we touched on, Patient Management Software (PMS) is a platform that automates routine administrative tasks for healthcare practices. Unlike Electronic Health Records (EHR) that focus on handling clinical data, PMS typically deals with scheduling, billing, patient communication and so on.
EHRs store medical records and track clinical information, while PMS focuses on the business side of healthcare. EHRs manage diagnoses, treatment plans, and patient history, whereas PMS ensures appointments, billing, and office operations run smoothly. Together, they create a complete solution for both patient care and practice management.
Missed patient appointments and inefficient scheduling disrupt workflows and cost practices thousands each year.
Paper charts or uncoordinated systems increase errors and slow down care.
Manual verification and claims handling can cause payment delays and extra administrative work.
Without a unified system, managing telehealth visits and remote monitoring is cumbersome.
Delayed results, limited portals, and inconsistent follow-ups make patients feel disconnected.
Manual processes make HIPAA and data security harder to maintain, raising legal and financial risks.
Here are 6 features you need to look for in your PMS.
Your PMS should simplify your practice’s appointment management. You’ll want features that reduce missed visits, send reminders automatically, and keep calendars up to date.
A PMS should simplify your billing and claims management, either with built-in tools or through integration with revenue cycle management system. Look for features that can verify insurance eligibility, submit claims electronically, and track payments.
Patients expect convenient access to their health information. A strong PMS should include a patient portal where they can view records, schedule visits and communicate securely with your practice.
A PMS works best when it communicates well with your Electronic Health Records. Integration with EHRs/EMRs allow free flow of relevant patient information between systems.
Seek customizable reports and dashboards in your PMS that let you monitor performance, track trends, and make informed operational decisions.
Patient data is sensitive and hence protected under several rules and regulations like HIPAA. Look for a PMS that offers encryption, access controls, audit trails, and regular updates to keep your practice compliant and secure.
So, with the must-have features in mind, here are five best patient management software solutions worth considering for your practice.
| Tool Name | Best Features | G2 Rating | Pricing |
| LeadSquared | Patient data consolidation, multichannel communication, AI-powered healthcare call center assistance | 4.5/5 | Pro: $60/user/month Super: $100/user/month |
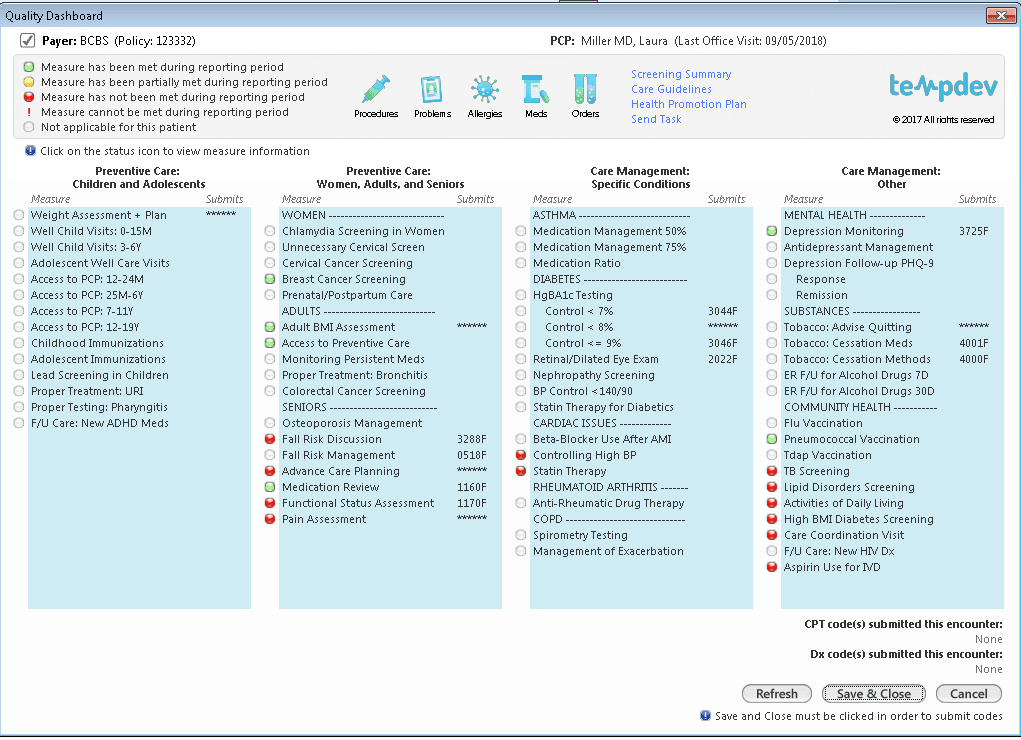
| athenaOne | AI-powered documentation, automated coding & billing, patient portal | 3.4/5 | Custom pricing |
| NextGen Healthcare | Unified scheduling & billing, specialty-specific messaging templates, mobile access | 3.8/5 | Custom pricing |
| Salesforce Health Cloud | Unified patient profiles, AI-powered analytics, real-time collaboration | 4.5/5 | Enterprise: $350/user/month Unlimited: $525/user/month |
| eClinicalWorks | Integrated scheduling & billing, AI-enhanced charting, telehealth support | 3.5/5 | $10,000 one-time or $599/month per provider; AI tools ~$100/month |
LeadSquared is a fully HIPAA-compliant, AI-powered Patient Management System designed to take the complexity out of running a healthcare practice. It centralizes patient records, appointments, billing, and communication in one platform, while automation handles the repetitive tasks that often slow teams down.
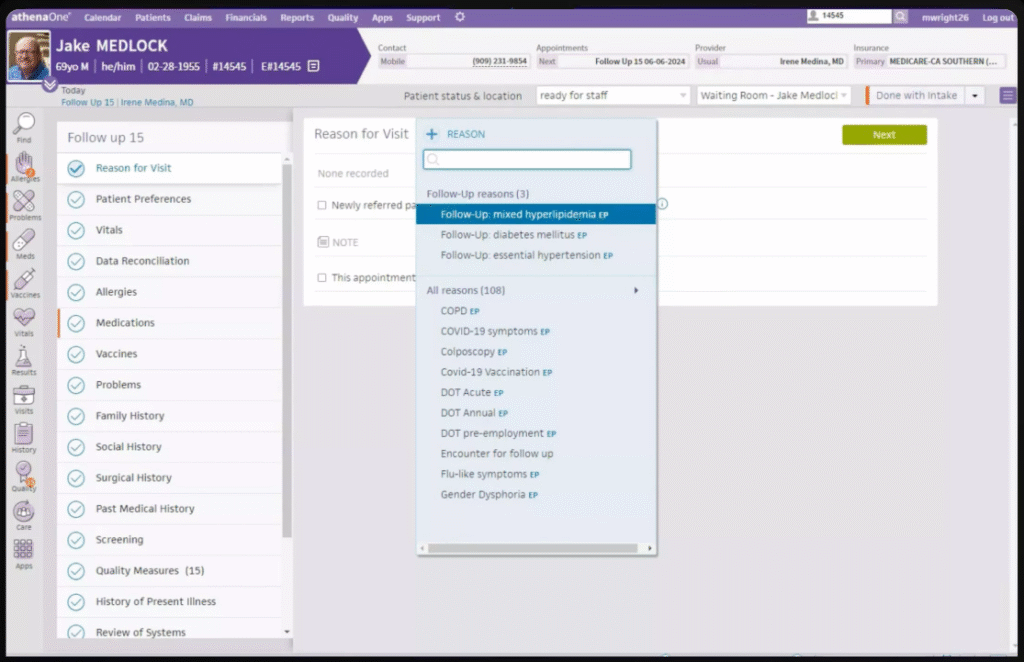
athenaOne is a cloud-based healthcare platform that combines EHR, medical billing, and patient engagement tools in one system. It uses AI to streamline documentation, reduce administrative work, and help practices focus more on patient care.
Custom pricing.
NextGen Healthcare is a cloud-based Practice Management System that helps small to mid-sized practices manage patients, scheduling, billing, and communication in one platform. It integrates with EHRs to streamline workflows and reduce administrative work, letting staff focus more on patient care.
Custom pricing.
Salesforce Health Cloud adapts the power of Salesforce’s well-known CRM to the needs of healthcare. It helps practices manage patient relationships, coordinate care across teams, and handle complex workflows while maintaining HIPAA compliance.
eClinicalWorks is an EHR-first platform with PRM features that extend its capabilities into patient management and CRM. It integrates scheduling, messaging, billing, analytics, telehealth, and clinical workflows into a single cloud-based platform.
A good Patient Management Software is an investment in efficient operations, happier patients, and stronger revenue. The best system is the one that aligns with your practice’s priorities, whether that’s scheduling, billing, or patient communication.
If you want all of this in one platform, with automation and AI built in, LeadSquared is a great choice.
Book a quick demo with LeadSquared to see how it can work for your practice.
An Electronic Health Record (EHR) is primarily about clinical care—storing and managing patient histories, test results, and prescriptions. A Patient Management System (PMS) handles the operational side: scheduling, billing, patient communications, and workflow automation. While EHRs keep medical data organized, PMS ensures the practice runs smoothly day-to-day. Many clinics use both together, and some PMS platforms, like LeadSquared, integrate with EHRs for a complete view.
Yes. Administrative challenges don’t disappear with size—missed appointments, billing delays, and communication gaps can hit smaller clinics harder because they have fewer staff. A PMS automates repetitive work, making a lean team more productive. It also ensures patients get reminders, updates, and better service, which directly improves retention and revenue.
Most PMS solutions send automated reminders by SMS, email, or push notifications. They also make rescheduling easier, so patients aren’t lost if something comes up. LeadSquared goes further by supporting WhatsApp reminders and AI-powered nudges, which improve attendance rates. Reducing no-shows means fewer gaps in the schedule and better financial stability for the practice.
Not typically. Modern PMS platforms are cloud-based, so practices don’t need servers or in-house IT teams. Pricing usually depends on practice size and features needed. While advanced features may cost more, the savings from fewer no-shows, faster billing, and reduced manual errors often offset the expense. LeadSquared, for example, offers tailored pricing, so practices pay for what they actually use.
Yes. A PMS centralizes all channels—calls, emails, SMS, and patient portals—so messages don’t get lost. Automated follow-ups ensure lab results, prescriptions, or reminders reach patients on time. LeadSquared adds multichannel capabilities, including WhatsApp, so practices can connect with patients where they are most active. Better communication leads to stronger patient relationships and satisfaction.
There is usually a learning curve, but most PMS platforms are designed to be user-friendly with dashboards and intuitive workflows. Vendors often provide onboarding and training support.
Yes. Many PMS tools integrate with telehealth platforms or have built-in virtual visit scheduling. This means appointments, notes, and billing for virtual care stay within the same workflow. Practices can manage in-person and telehealth patients seamlessly, track outcomes, and ensure proper reimbursement. Having telehealth inside the PMS also helps with follow-ups and remote patient engagement.
PMS systems streamline billing by automating claim submission, checking for errors before sending, and tracking rejections or denials. This reduces manual effort and improves cash flow. Some platforms handle this directly, while others, like LeadSquared, integrate with billing and insurance systems for smoother processing. By reducing errors, practices cut down on revenue leakage.
Yes, if you choose a HIPAA-compliant vendor. Reputable PMS providers use encryption, secure cloud hosting, and audit trails to protect sensitive data. Access controls ensure only authorized staff see patient information. Many systems also log activity for compliance reporting. LeadSquared and other top PMS vendors make security a top priority, so practices stay protected from breaches.
Start with your pain points—do you need better scheduling, faster billing, or improved patient engagement? Then compare features, ease of use, integrations, and cost. Smaller practices may value simplicity, while larger ones need scalability. If you want a PMS that’s customizable, integrates well with EHRs, and uses AI to automate repetitive work, LeadSquared is a strong candidate.
Yes. While EHRs capture medical details, many PMS platforms now include reporting and analytics that track appointments kept, treatment adherence, and follow-ups completed. This data helps practices identify gaps in care and intervene early. Some systems also allow outcome dashboards that connect to clinical data, giving providers a more complete picture of patient progress.
For practices with more than one location, a PMS centralizes scheduling, records, and billing across sites. Staff can access shared patient data without duplication, and management gets a unified view of operations. LeadSquared, for example, offers customizable workflows and multi-branch reporting, making it easier to track performance and coordinate care across multiple clinics.
Yes. Many PMS solutions connect with CRMs, email tools, or marketing platforms to help practices attract and retain patients. This can include automated campaigns, satisfaction surveys, or recall reminders. LeadSquared stands out here, since it combines patient management with CRM-like engagement features, allowing practices to nurture stronger, long-term patient relationships.
Definitely. Most modern PMS platforms offer templates and workflows tailored to specialties like dentistry, dermatology, or behavioral health. This ensures that scheduling, documentation, and billing codes fit the specific practice type. Some vendors allow deep customization, so providers can fine-tune the system to their exact workflows, rather than forcing a one-size-fits-all model.
1
2. Do small practices really need a PMS?
Yes. Administrative challenges don’t disappear with size—missed appointments, billing delays, and communication gaps can hit smaller clinics harder because they have fewer staff. A PMS automates repetitive work, making a lean team more productive. It also ensures patients get reminders, updates, and better service, which directly improves retention and revenue.
3. How does a PMS help reduce no-shows?
Most PMS solutions send automated reminders by SMS, email, or push notifications. They also make rescheduling easier, so patients aren’t lost if something comes up. LeadSquared goes further by supporting WhatsApp reminders and AI-powered nudges, which improve attendance rates. Reducing no-shows means fewer gaps in the schedule and better financial stability for the practice.
4. Is a PMS expensive to maintain?
Not typically. Modern PMS platforms are cloud-based, so practices don’t need servers or in-house IT teams. Pricing usually depends on practice size and features needed. While advanced features may cost more, the savings from fewer no-shows, faster billing, and reduced manual errors often offset the expense. LeadSquared, for example, offers tailored pricing, so practices pay for what they actually use.
5. Can a PMS improve patient communication?
Yes. A PMS centralizes all channels—calls, emails, SMS, and patient portals—so messages don’t get lost. Automated follow-ups ensure lab results, prescriptions, or reminders reach patients on time. LeadSquared adds multichannel capabilities, including WhatsApp, so practices can connect with patients where they are most active. Better communication leads to stronger patient relationships and satisfaction.
6. Will my staff need a lot of training to use a PMS?
There is usually a learning curve, but most PMS platforms are designed to be user-friendly with dashboards and intuitive workflows. Vendors often provide onboarding and training support.
7. Can a PMS help with telehealth?
Yes. Many PMS tools integrate with telehealth platforms or have built-in virtual visit scheduling. This means appointments, notes, and billing for virtual care stay within the same workflow. Practices can manage in-person and telehealth patients seamlessly, track outcomes, and ensure proper reimbursement. Having telehealth inside the PMS also helps with follow-ups and remote patient engagement.
8. How does a PMS handle billing and insurance claims?
PMS systems streamline billing by automating claim submission, checking for errors before sending, and tracking rejections or denials. This reduces manual effort and improves cash flow. Some platforms handle this directly, while others, like LeadSquared, integrate with billing and insurance systems for smoother processing. By reducing errors, practices cut down on revenue leakage.
9. Is a PMS secure enough for patient data?
Yes, if you choose a HIPAA-compliant vendor. Reputable PMS providers use encryption, secure cloud hosting, and audit trails to protect sensitive data. Access controls ensure only authorized staff see patient information. Many systems also log activity for compliance reporting. LeadSquared and other top PMS vendors make security a top priority, so practices stay protected from breaches.
10. How do I choose the right PMS for my practice?
Start with your pain points—do you need better scheduling, faster billing, or improved patient engagement? Then compare features, ease of use, integrations, and cost. Smaller practices may value simplicity, while larger ones need scalability. If you want a PMS that’s customizable, integrates well with EHRs, and uses AI to automate repetitive work, LeadSquared is a strong candidate.
11. Can a PMS help track patient outcomes?
Yes. While EHRs capture medical details, many PMS platforms now include reporting and analytics that track appointments kept, treatment adherence, and follow-ups completed. This data helps practices identify gaps in care and intervene early. Some systems also allow outcome dashboards that connect to clinical data, giving providers a more complete picture of patient progress.
12. How does a PMS support multi-location practices?
For practices with more than one location, a PMS centralizes scheduling, records, and billing across sites. Staff can access shared patient data without duplication, and management gets a unified view of operations. LeadSquared, for example, offers customizable workflows and multi-branch reporting, making it easier to track performance and coordinate care across multiple clinics.
13. Does a PMS integrate with marketing or patient engagement tools?
Yes. Many PMS solutions connect with CRMs, email tools, or marketing platforms to help practices attract and retain patients. This can include automated campaigns, satisfaction surveys, or recall reminders. LeadSquared stands out here, since it combines patient management with CRM-like engagement features, allowing practices to nurture stronger, long-term patient relationships.
14. Can a PMS adapt to specialty-specific needs?
Definitely. Most modern PMS platforms offer templates and workflows tailored to specialties like dentistry, dermatology, or behavioral health. This ensures that scheduling, documentation, and billing codes fit the specific practice type. Some vendors allow deep customization, so providers can fine-tune the system to their exact workflows, rather than forcing a one-size-fits-all model.