- Home
- Learn
- Healthcare
- Meeting the New Demands of Patient-Centered Healthcare
HEALTHCARE
Meeting the New Demands of Patient-Centered Healthcare
Contents
Let’s play Jeopardy—briefly. The contestant chooses healthcare for $1000.
The host reads the answer…
Providing care that is respectful of, and responsive to, individual patient preferences, needs, and values, and ensuring that patient values guide all clinical decisions.
Ding! The contestant answers…
What is patient-centered care?
Correct. (The definition comes from the Institute of Medicine).
Okay, TVs off, please. It’s time to read.
NEJM Catalyst reiterates what we learned from our quick visit to the long-running gameshow…
“In patient-centered care, an individual’s specific health needs and desired health outcomes are the driving force behind all health care decisions and quality measurements.”
They add this important idea:
“Patients are partners with their health care providers, and providers treat patients not only from a clinical perspective, but also from an emotional, mental, spiritual, social, and financial perspective.”
Success depends on a partnership between individuals and their healthcare providers. The individual’s needs and aspirations drive both healthcare decisions and how outcomes are measured.
The objective of patient-centered healthcare is to make patients more engaged, and therefore, more satisfied with the delivery of their care. And the hope is efficacy increases.
We’ll stick with NEJM Catalyst here to examine the benefits of patient-centered care.
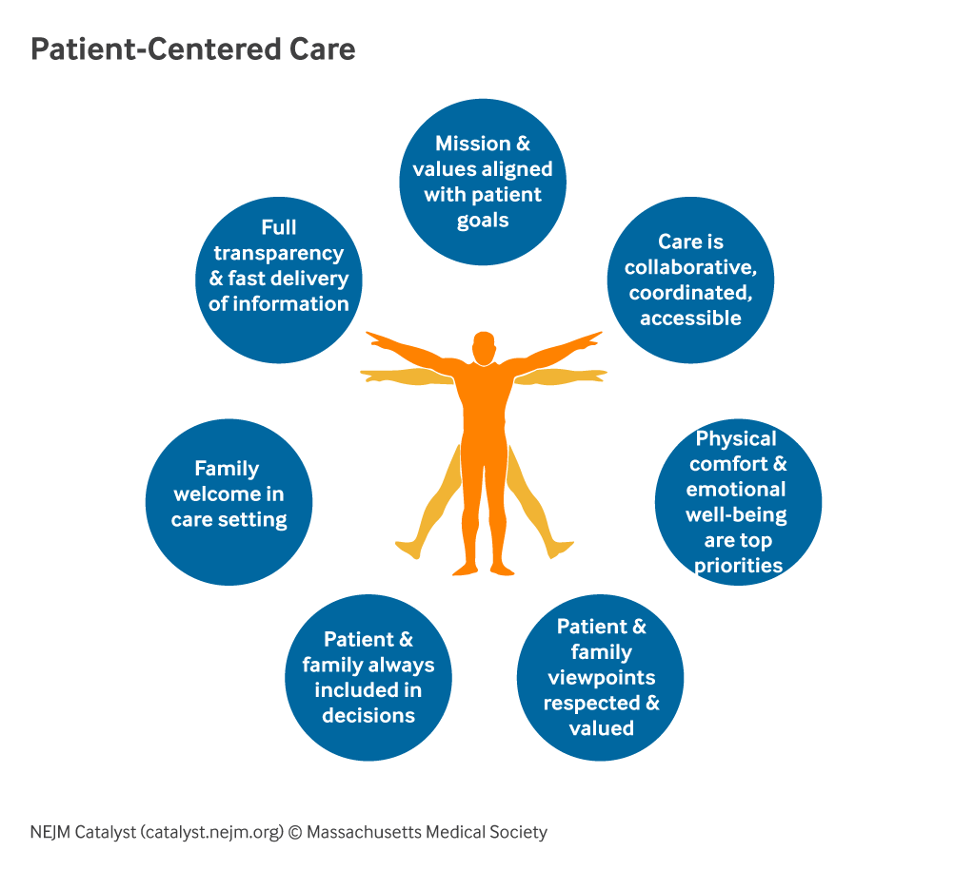
Starting at 12 o’clock in the image above, seven elements are revealed:

HealthLeads attempts to simplify patient-centered care with four C’s: culture, care, communication, and collaboration.
According to Welkin Health, four evidence-based benefits of patient-centered healthcare serve patients and providers alike.
Research from AMA Journal of Ethics claims that when patient values and preferences are prioritized, they engage more in treatments, which results in better health outcomes. Practices are able to:
Patient-centered care increases patient satisfaction. The patient’s active participation drives the care plan and gives clinicians a clearer idea of how to exceed their expectations.
Obviously, you can no longer ignore your practice’s reputation as shared via online media channels. With patient-centered care models, more patients feel they’re being taken care of properly and more safely.
Patient-centered care has proven to increase staff morale and job satisfaction. When clinicians feel they work at a healthcare organization focused on patient-specific needs, they are more likely to feel satisfied with and less likely to feel burnout.
Offer appointment options that are easy to schedule. Also, ensure the referrals you provide to accessible specialists are clear. Finally, be sure patients that can’t travel to your location are informed about available transportation options.
Understand the evolving integrative health care landscape your patients live in. Consider botanical medicine remedies, pain management options, and any religious or cultural values patients have.
Actively participate in and understand your patient’s care plan. Be flexible when coordinating front-line patient care, clinical care, ancillary care, and support services. Ensure every clinician remains informed about each step in the patient’s care.
Help your patients feel in control of their care. Motivate them to follow the care plan by respecting their need for information. Provide thorough information regarding their clinical status, progress and prognosis, care processes, and autonomous self-care.
When patients are physically comfortable and calm, they’re likely to be more willing to discuss their pain management options their assistance needs. Do what you can to reduce anxiety and ensure patients you have their best interests at heart. Address any anxieties they express regarding their status, prognosis, or treatment.
It’s vital to accommodate the family and close friends your patients trust and involve them in the decision-making. Explain your care plan to them so they can participate—and help. Let caregivers know you recognize their needs and will act as a trusted consultant and supporter.
Patient-centered care doesn’t end when the patient goes home. Make sure the patient’s family and caretakers understand the patient’s physical limitations, dietary requirements, and medication schedules. Ensure they’re informed about access to physical, financial, clinical, and social resources related to the treatment plan.
“We’re seeing a huge appetite from patients to interact with us digitally and connect with care. We’ve shifted the paradigm from reactive — answering when a patient calls us — to proactive and engaging patients when we can see that they need care. We’re developing a unified strategy to orchestrate the patient’s journey across a lifetime of care and thousands of patients are already seeing the impact.”
Lisa Yerian, MD, Chief Improvement Officer at Cleveland Clinic
How is Cleveland Clinic executing in its effort to accomplish what Dr. Yerian said?
In short, the answer is by integrating its EHR system with CRM.
“As Epic is our clinical record of truth, the CRM system is our engagement record of truth. Anytime you can think of consistent engagement, that’s where you can see the CRM system coming into play,” says Beth Meese, Executive Director of Digital Health & Enterprise CRM at Cleveland Clinic.
You’ll want to learn more about the role HIPAA-compliant CRM plays in delivering a new patient-centric approach to healthcare, but above all, understand:
CRM represents a centralized and automated way to gather and track patient engagement data. Every caregiver can access the information needed to create the highest quality, most personalized, and compassionate experience for the patient.