- Home
- Learn
- Healthcare
- The Future of Healthcare Consumerism: Trends, Data, and Insights
HEALTHCARE
The Future of Healthcare Consumerism: Trends, Data, and Insights
Contents
Healthcare consumerism places the patient at the center. Patients are empowered to engage with their providers and make decisions about their health.
We call it the “patient-first” approach.
According to Privia Health, the three foundational aspects of providing great patient care call for doctors:
The article I cited above lists a series of trends as important factors in the future of healthcare consumerism:
90% of Gen Z and 87% of millennial patients researched healthcare costs prior to visiting their physician for services.
SOURCE
When it comes to examining healthcare today and prognosticating about its future, there’s no shortage of data. And while it comes from many different angles, much of it intersects in a somewhat obvious way and precipitates a clear path forward.
I believe we can agree on these notions:
You need to put the patient at the center of every decision and develop market and growth strategies based on the segments you serve. Let’s unravel this…
Healthcare Consumer Market Report, a study by Huron, reveals the following findings:
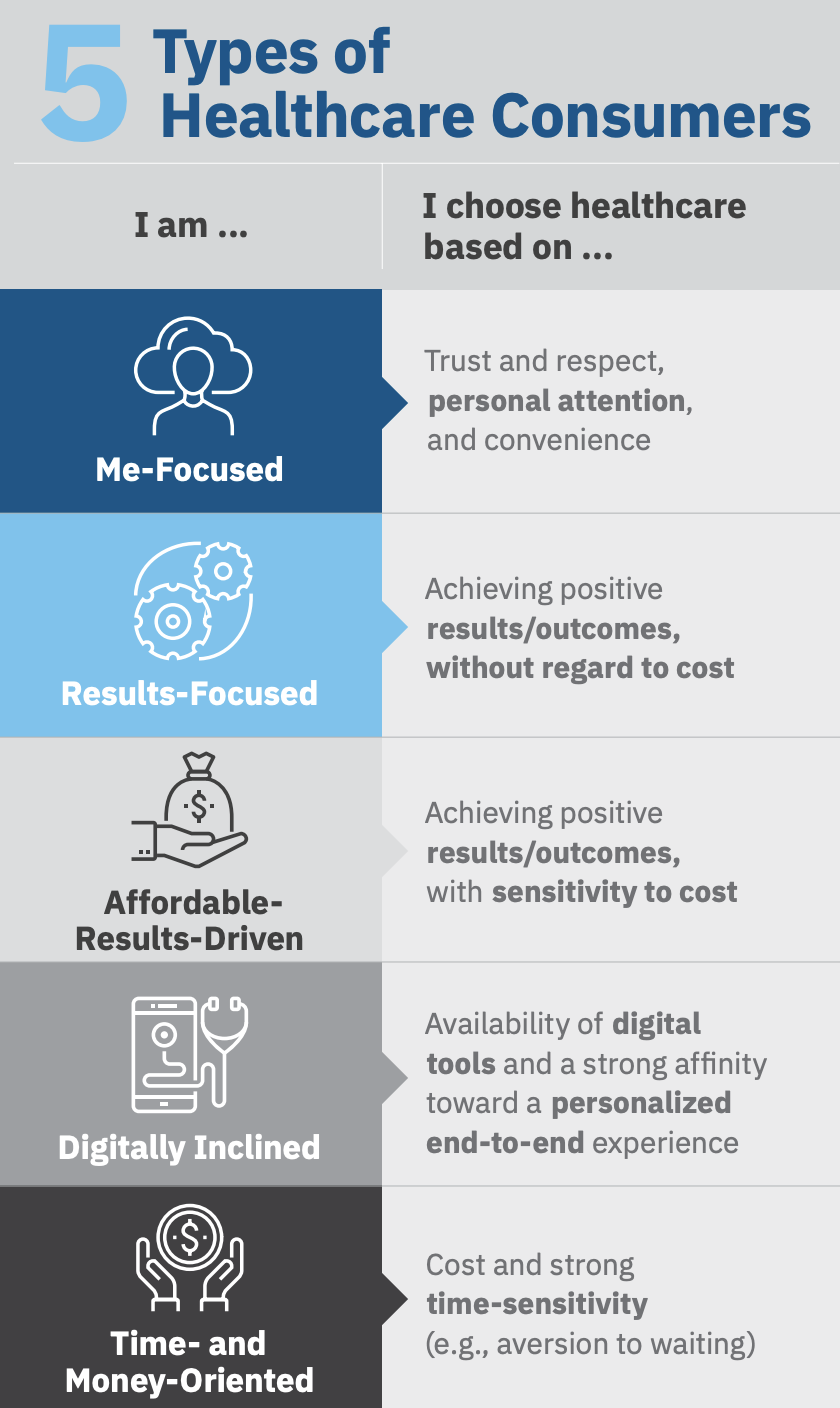
Huron research claims there are five distinct types of healthcare consumers. While not everyone has “perfect vision” when it comes to examining their healthcare options, consumers choose healthcare services based on a combination of attitudes and preferences related to satisfaction, quality, convenience, and personalization.
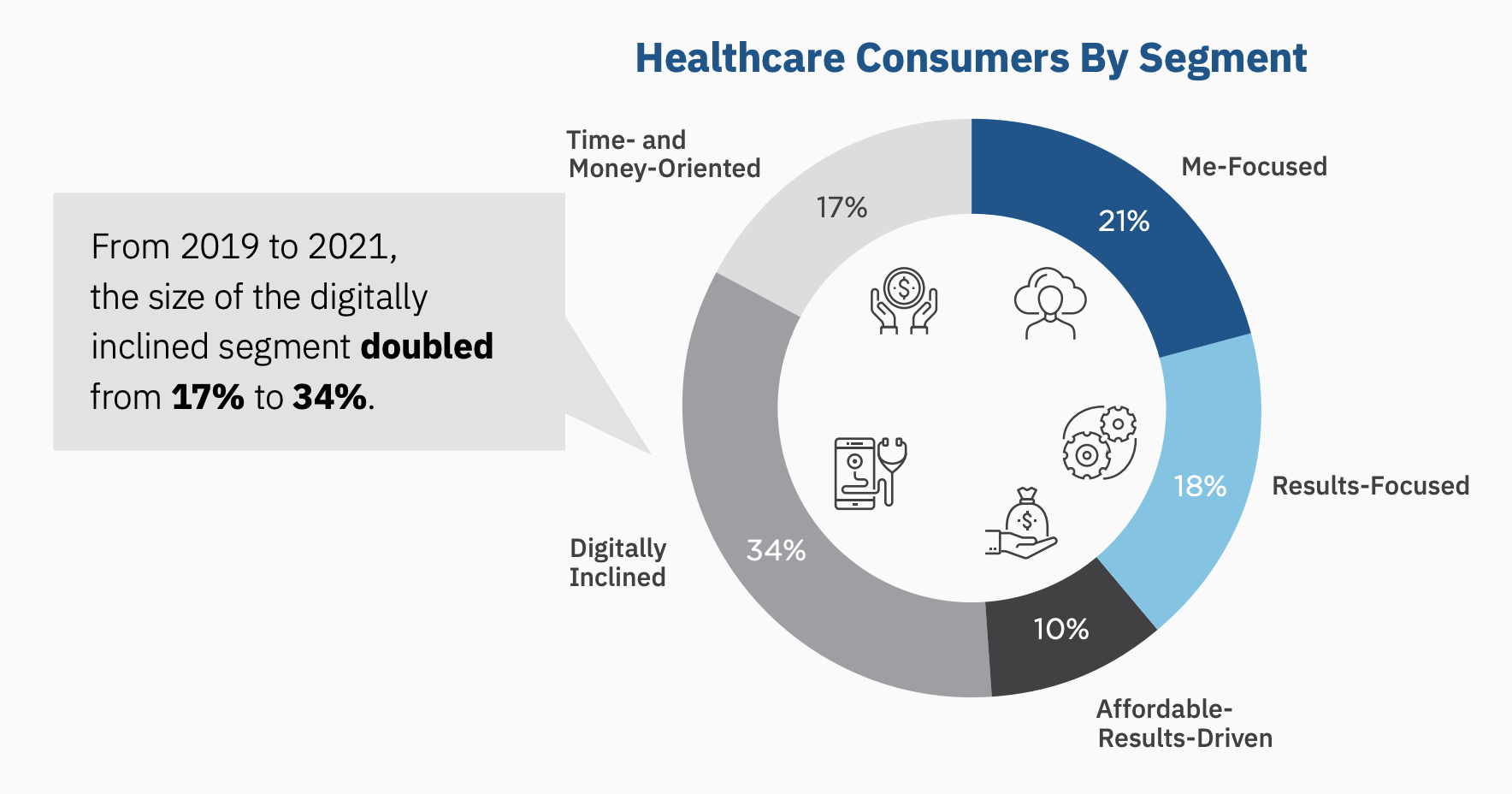
The “digital inclined” segment is the largest slice of the piece. Such consumers value online quality ratings, reviews, and comparison tools.
Wearable devices paired with remote patient monitoring and virtual care present a significant opportunity to change the foundation of care delivery. It follows that healthcare organizations able to figure out how to monitor data collected from wearables and other digital devices and use it to proactively address health issues will be able to:
“The challenge will be developing and delivering on consumer priorities in organizations where a ‘consumer first’ mindset has not traditionally guided strategy,” write the authors of the Huron report.
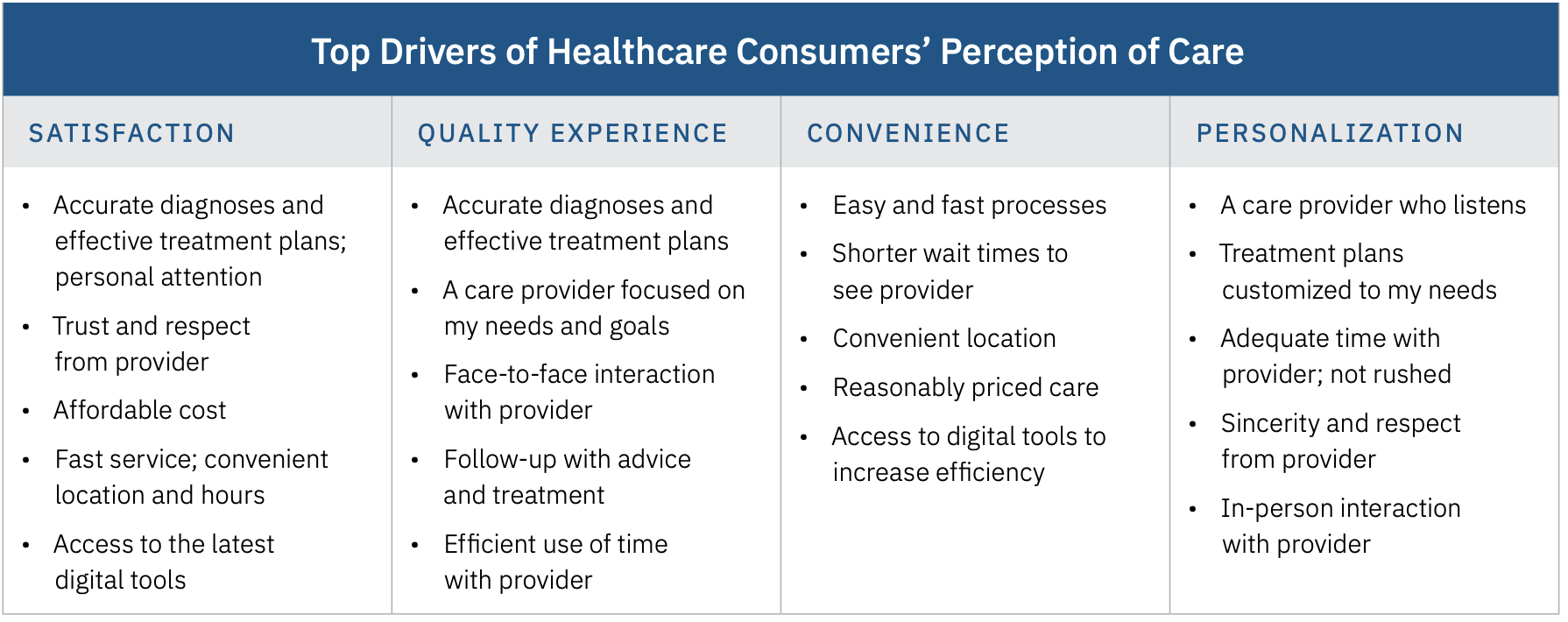
Huron claims the data suggests organizational transformation must center on consumer preferences related to how they choose healthcare and engage with health systems and providers.
Building a consumer-centric healthcare organization requires a deep understanding of your consumer base and must be driven by data and analytics.
The research reveals satisfaction is high and loyalty is not. Nearly 75% of consumers surveyed in 2019 and 2021 report being satisfied with the healthcare they receive, but nearly half say they are willing to make a change if presented with the right driver.
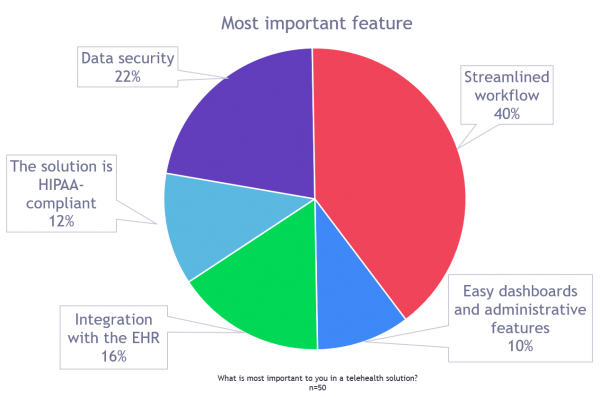
EHR provider Greenway Health surveyed 50 clients in 2021 and found telehealth helped its clients manage COVID-19 visits and has grown immensely to include behavioral health visits, prescription refills, and far more. They report no practices plan to decrease their use of telehealth and they are perfectly comfortable making it part of their patient care.
They asked their clients, “What is the most important feature when adopting a telehealth solution?”
Virtual primary care now plays a vital role in the healthcare ecosystem. But look at these alarming statistics:
What gives? Patients have grown weary of time-consuming doctor appointments that are cold and impersonal. In 2020, the average wait time for a new patient to get an appointment with a family doctor was 29 days, according to Consumer Reports on Health.
Virtual care offers the prospect of delivering a more compassionate experience that is respective of the patient’s time. And the numbers reveal how important it can be to have a PCP.
Here’s what Included Health (cited above) has to say:
“Virtual primary care offers the access and convenience of telemedicine, but pairs those aspects with the benefits of traditional primary care. Patients receive an integrated view of their health, and receive continuity of care with the same physician, which is done virtually via video visits.”
I’d be remiss to not also mention virtual primary care offer patients the ability to easily schedule an appointment with their PCP. And patients can see their physician wherever and whenever it’s most convenient (as opposed to the other way around).
The Centers for Disease Control and Prevention (CDC) claims that 20% of Americans have mental health concerns. 16 million adults in the U.S had at least one major depressive episode in 2020.
Clearly, behavioral health must be a top concern for the entire ecosystem of individuals, families, employers, health plans, and providers.
Unsurprisingly, most people prefer to be treated for their mental health issues in the privacy of their homes. Doctors absolutely must understand the need for privacy and providers must comply with HIPAA regulations out of respect for their patients.
Though it may sound cliché, it’s transformation time. Thriving in A Changed Healthcare Market, a research report from Huron, presents the following findings:
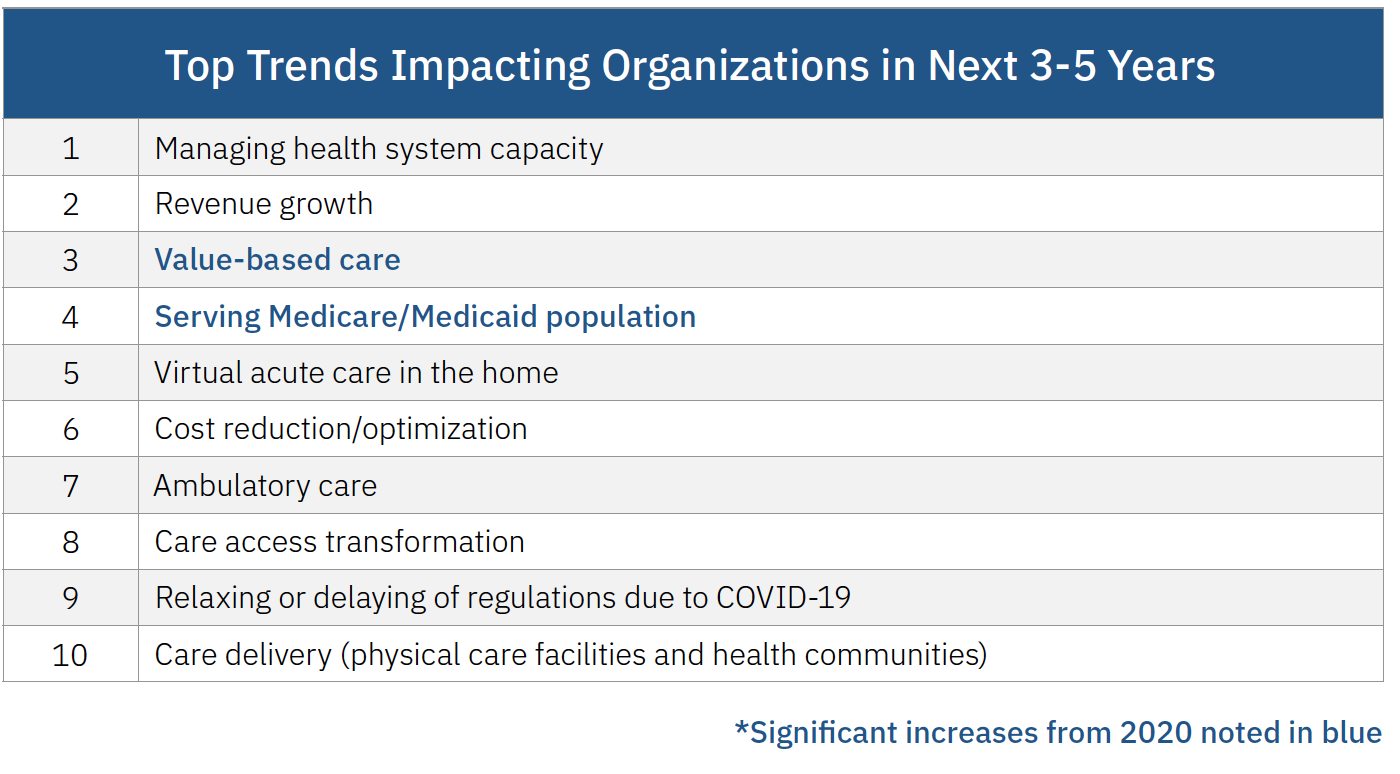
Executives claim managing system capacity has the highest organizational impact, followed by revenue growth, value-based care, and serving Medicare and Medicaid populations. Creating the efficiencies needed for breakthrough improvement in cost and quality will call for reconsidering cost structures, care delivery models, reimbursement, and financial strategies.
Healthcare organizations must now implement technology-driven initiatives to optimize core functions and business systems.
Additionally, building better, more secure data structures and advancing the use of analytics for decision-making are vital to tackle challenges that range from consumerism to cost management and care delivery.
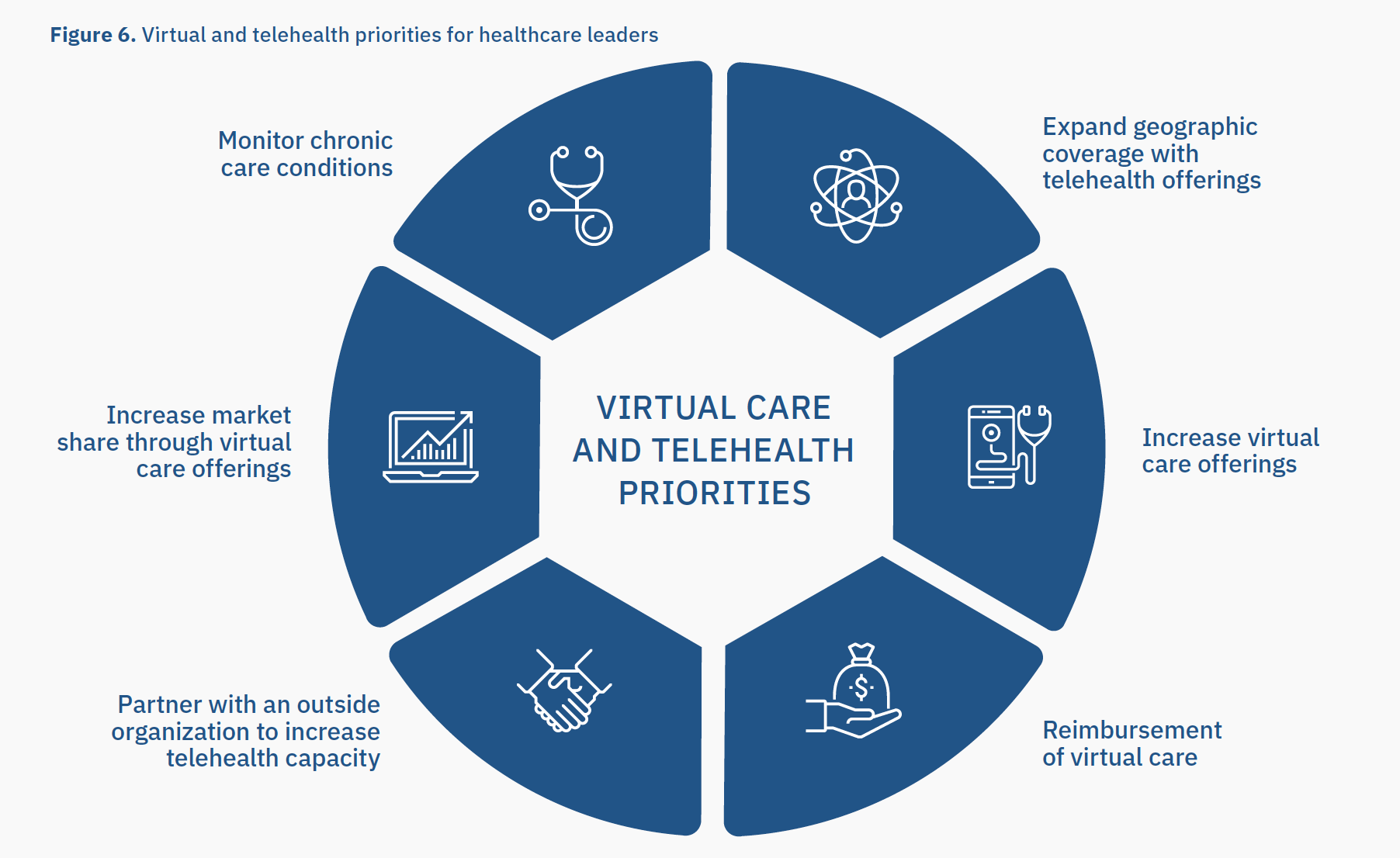
Leaders’ challenges call for managing system capacity, changing care delivery models, expanding virtual care and improving care access. The growth strategies shown above focus on technology-enabled care and building integrated care delivery models.
The challenge here and now: deliver the right balance of in-person and virtual care. To thrive going forward in the 20s calls for true cost transformation and making consumer-driven transformation central to your growth strategies.